Introduction
More than 17,000 patients yearly require a tracheostomy in the United Kingdom,1 with 400-500 of these occurring within National Health Service (NHS) Wales.2 Whilst an essential procedure, patients often have multiple comorbidities and complex care needs, which impact on ongoing tracheostomy care and weaning options. Approximately 20-30% of patients with a tracheostomy will experience measurable harm resulting in hospital or intensive care unit (ICU) readmission, prolonged in-patient stays, significant morbidity, and even death.3 Staff caring for these patients often report low confidence regarding routine tracheostomy care and managing emergencies associated with blocked or displaced tracheostomy tubes.4
The importance of education in tracheostomy care and emergency management is well recognised, with several studies demonstrating direct improvements in patient outcomes following the implementation of training programmes.5–7 However, there is wide variation in the provision of training among and between specialties, hospitals, and community settings. Most tracheostomy training involves face-to-face training, thus presenting significant demands for staff to be released from clinical roles and involving significant amounts of time to travel to appropriate training facilities.4 The COVID-19 pandemic compounded these issues, with a surge in patients requiring tracheostomy.8 Significantly more healthcare professionals required training at a time when training provision was severely hampered by clinical demands, inability to collocate staff, and the closure of training facilities.
In response to these demands, we developed and implemented a national digital toolkit “TRACHES” across all acute hospitals in Wales with the aim of raising educational standards for tracheostomy care. In this short report, we describe the TRACHES toolkit, the deployment strategy, and its adoption across Wales.
Methods
Target Population
The target population comprised all healthcare professionals caring for patients with a tracheostomy in acute district general and tertiary hospitals across Wales. Healthcare in Wales is organised into seven health boards (HB), which manage both primary and secondary care. There are 14 acute hospitals with critical care units covering six out of the seven HB (no acute hospitals in the remaining HB).
Implementation Framework
The Simple Implementation Science (SIMPSI) framework9 was utilised to provide a formal governance structure for content creation, curation, and deployment. The SIMPSI framework was created by the Institute for Clinical Science and Technology (ICST) and has previously been proven to be an effective implementation framework.10 The approach utilises 4-key stages: 1) development – scoping, innovation development, and early optimisation; 2) instillation – installing the innovation into a test environment; 3) scaling – formally introducing the innovation into the system and maximising uptake; and finally, 4) sustainability - where the innovation becomes part of the system, it is widely adopted and accepted (Figure 1).
The approach also recognises the importance of enablers, or key principles, which must be in place prior to moving through the phases. These enablers include the implementation team, organisational structures, identification of target and power (influencers) layers, alignment, and fidelity.
‘TRACHES’ Toolkit Development
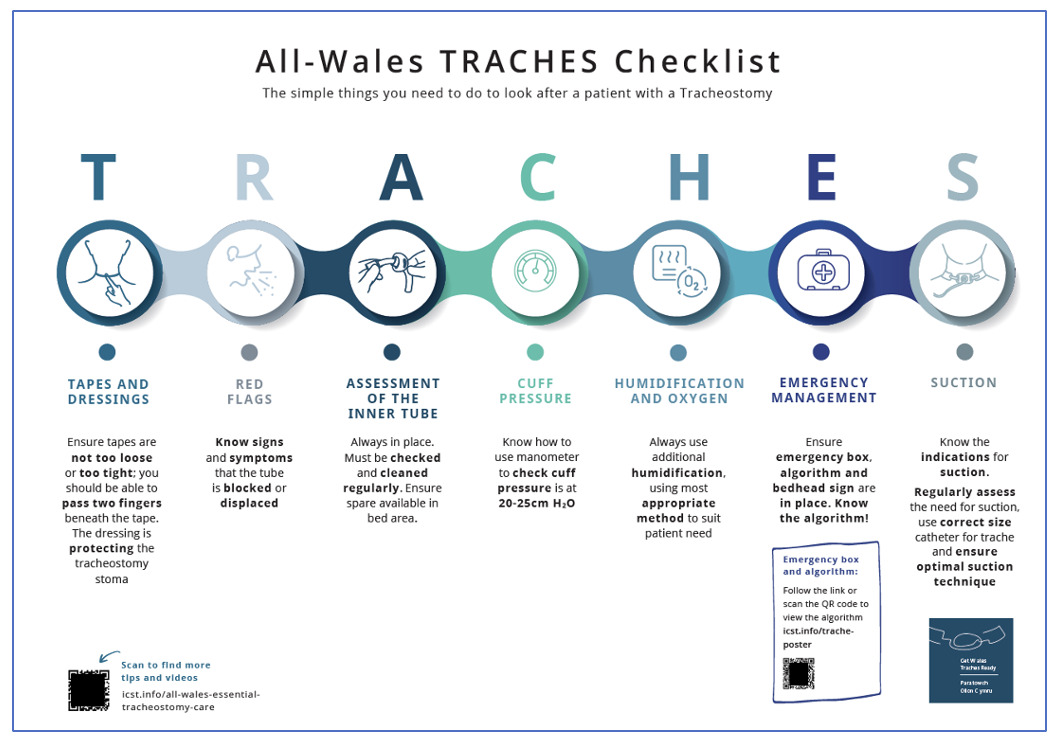
Tracheostomy care was broken down into modules dealing with key aspects of safe tracheostomy management. The acronym ‘TRACHES’ was chosen to reflect 7-key aspects, which were Tapes and dressings; Red flags; Assessment of inner tube; Cuff pressure management; Humidification and oxygen therapy; Emergency management; and Suction. Leading experts across NHS Wales (including consultants in Intensive Care Medicine, ear nose & throat surgeons, oro-maxillofacial surgeons, specialist nursing staff, physiotherapists and speech and language therapists) and the National Tracheostomy Safety Project (NTSP) were involved in the development of educational content for these components via short (3-5 minute) videos. The content is hosted on a single digital platform requiring user registration and includes the individual components of the TRACHES toolkit, tutorials, a Checklist poster (see Figure 2), case-based assessments, certification, NTSP resources, and webinars on the topics.
‘TRACHES’ toolkit Implementation
The ‘TRACHES’ toolkit was implemented in August 2020 across all 14 acute hospitals with critical care units. Implementation was achieved using The ICST framework. The Implementation Team, comprising implementation experts from ICST and tracheostomy leaders from hospitals in NHS Wales (from variety of clinical backgrounds, but included medical staff, specialist nurses, physiotherapists and speech and language therapists), used Implementation Science methodologies9 to scale the toolkit nationally. The team sought alignment and collaboration with stakeholder groups across the tracheostomy healthcare environment, considering the possible patient journey through a hospital’s departments. Stakeholders were appropriately engaged at each phase of the implementation via an existing network in NHS Wales and direct contact from the project clinical lead. This process ensured that the value of the project was clearly relayed, which is a pivotal component of ICST’s implementation science approach. This approach is designed to empower staff to utilise toolkits to raise the standard of care across their teams, reducing variation and inequality through a digital behaviour change system.
Data Collection
Uptake of the ‘TRACHES’ toolkit was determined by evaluating registration and completion of certification data from the ICST platform at an individual, departmental, hospital, and health board level. Access to educational resources and competency assessments were recorded.
Statistics
Analysis was performed using descriptive statistics for interactions with the ‘TRACHES’ toolkit. This was performed utilising in-build reporting mechanisms within the toolkit.
Results
Implementation Uptake
Since its launch in August 2020, healthcare staff from 14 acute hospitals have accessed the ‘TRACHES’ toolkit. By the end of September 2023, content had been accessed 19,183 times by nursing staff (69.6%), Allied Healthcare Professionals (20.3%), medical staff, healthcare support workers, and students, with nine hundred and seventy-six unique users averaging 19 page visits per user, demonstrating comprehensive engagement with the multimedia resources on the platform. Four hundred and seventy-one healthcare professionals completed the integrated competency assessment (73.0% nursing, 19.0% Allied Healthcare Professionals (Figure 3)).
Discussion
Our study has shown that it was possible to deploy a high-quality educational resource at scale and pace. We utilized a digital system that has had proven success in implementing solutions at a national level in response to a variety of clinical needs.10,11
Previous work within NHS Wales demonstrated the effectiveness of a single-site QI programme, with a significant focus on delivering education, resulting in reductions in adverse events and length of stay.2 Similarly, McGrath and colleagues demonstrated the potential to implement a tracheostomy quality improvement programme across multiple sites.1,7 Twenty UK sites implemented up to 18 guided improvement interventions, with a clear focus on education and patient safety, resulting in improved outcomes.1 This approach may not be generalisable however, as sites were highly motivated, had executive-level support, were intensively mentored by project leadership, and accessed a nationally recognised training programme. Our challenge was creating behaviour change at a national scale without traditional support mechanisms such as extra resources.
The digital platform (allwales.icst.org.uk) to which 13,000 healthcare professionals are signed into in Wales allows rapid dissemination of education, including updates when available. Furthermore, data on the site and profession of signatories allowed targeting of resources to hospitals or locations, including identifying areas of high and low usage. This ensured uptake across all acute hospitals within NHS Wales as well as a clear focus on provision to the entire multidisciplinary team.
Limitations
We acknowledge that we are currently only reporting here on the development and deployment of a novel educational toolkit, and not on patient outcomes associated with access to education. This next stage is in progress but requires the implementation of a national database to ensure complete data collection. Through this process, we aim to determine the toolkit’s impact specifically frequency and severity of adverse events more fully e.g., accidental dislodgements, wound infections etc., as well as impact on key weaning outcomes e.g., time to cuff deflation, time to decannulation. It will allow potential project expansion to support and evaluate local and national quality improvement programmes. The Toolkit is also undergoing further updates with the potential to make it available across the entire NHS in the UK. Additionally, we recognise that the Toolkit is focused on adult patients within hospital care. Future developments are now underway to support healthcare staff caring for adult patients living within community settings, as well as paediatric patients across health and social settings. Options for utilisation of immersive technologies to support implementation are also being considered, with utilisation of the TRACHES algorithm being used as part of parallel workstreams and feasibility trials.11,12
Conclusion
We report on the outcomes of implementing a national training program, ‘TRACHES’, across all acute hospitals in Wales. We note widespread uptake across various professional groups. We propose that the TRACHES toolkit is a potential model to improve tracheostomy care at a population level.
Author Contributions
All authors were involved in the literature search, study design, manuscript preparation and manuscript review. PT and CD were also involved in the data collection, and PT completed the data analysis.
Conflict of Interest
No authors have any conflicts of interest.
Funding
The Welsh Government funds the Respiratory Health Implementation Group (RHIG), of which Simon Barry is the national clinical lead. RHIG funds The Institute of Clinical Science and Technology, which creates and implements the TRACHES toolkit for NHS Wales.
_framework.png)


_framework.png)