Introduction
Tracheostomy is widely used to support patients with respiratory failure or airway obstruction,1–5 but the implications for care remain underexplored. Each year, approximately 250,000 adults undergo tracheostomy, many with underlying conditions such as cancer, neuromuscular diseases, and genetic disorders.6–8 Around 4,000 pediatric tracheostomies are performed annually, emphasizing cross-generational needs.9 While tracheostomy plays a vital role in maintaining respiration, it also introduces complex challenges for patients, caregivers, and healthcare professionals due to risk of adverse events, communication barriers, and the psychological burden associated with chronic airway management.10–14 Patients with tracheostomy also have increased risk for airway infections and reduced quality of life,15–17 with fears around self-efficacy in maintaining a safe airway.17 As team leaders in airway management, communication, and tracheostomy care, nurses, speech language pathologists, respiratory therapists, and physicians require deeper insights into these lived experiences.18
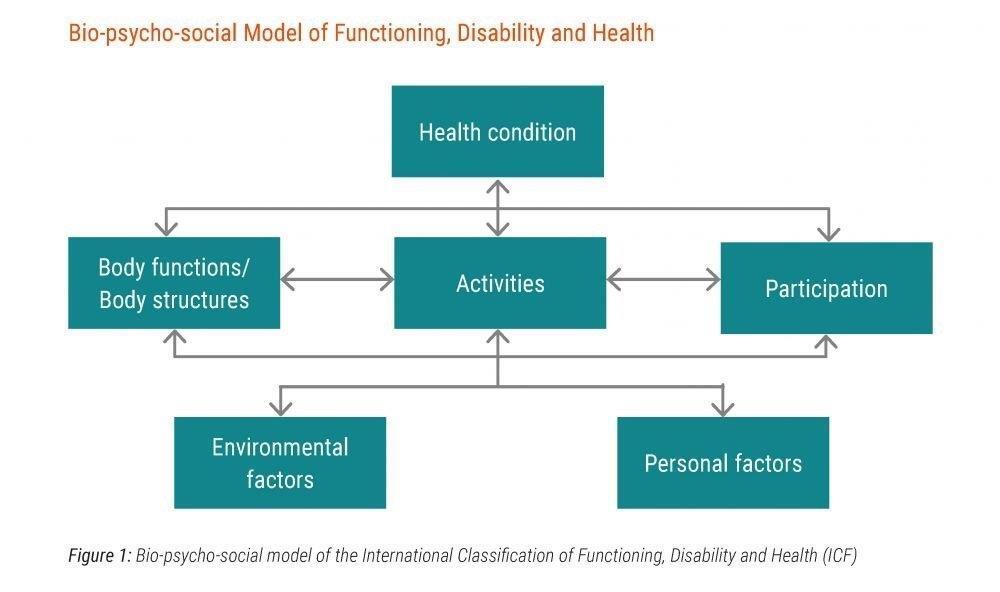
Tracheostomy care in the community introduces an additional layer of complexity, requiring coordinated support from family members, home health nurses, and interprofessional healthcare team members.4,6,19–23 Care partners report several barriers, from coordinating complex care in non-clinical settings to securing access to necessary medical equipment.24–27 Such challenges are amplified during healthcare crises, supply chain shortages, or economic downturns. The literature on tracheostomy emphasizes clinical outcomes, with far less attention to how patient and caregiver experience and social context shapes these outcomes.28 As a result, clinical leaders overseeing tracheostomy teams need to better understand and address these considerations.29 The biopsychosocial model highlights the complex interactions between physiological health, psychological factors, and social support, allowing multifaceted insights into experiences of tracheostomy patients and their caregivers.30
This study aims to bridge this gap in understanding tracheostomy care by exploring the lived experiences of individuals with tracheostomies, their caregivers, and healthcare professionals. By examining the key challenges, needs, and supports necessary to improve quality of life and care, this research can improve communication, understanding, and management of unmet care needs. Specifically, it seeks to answer: What are the primary challenges and support requirements faced by individuals with tracheostomies, their caregivers, and healthcare professionals in managing tracheostomy care? Through qualitative analysis of narratives from a diverse group of participants, this study aspires to inform the design of patient-centered, inclusive healthcare approaches that address the social and emotional dimensions of tracheostomy care.
Methods
Qualitative Approach and Research Paradigm
This study uses a phenomenological approach within a constructivist-interpretivist paradigm to explore the subjective experiences of individuals with tracheostomies, their caregivers, and healthcare professionals.31,32 Guided by the International Classification of Functioning, Disability, and Health (ICF) framework, it applies a biopsychosocial model to examine the interaction of physical, environmental, and personal factors affecting functioning and quality of life.30,33,34 This framework emphasizes contextual influences on health outcomes and daily activities, capturing the psychosocial challenges of tracheostomy care.35–37 By framing experiences holistically, the study aligns with the goals of phenomenological inquiry.38
Researcher Characteristics and Reflexivity
The research team, consisting of experienced qualitative researchers and healthcare professionals specializing in tracheostomy care, employed strategies to maintain reflexivity and minimize bias. Regular discussions and reflexive journaling were used to identify and set aside preconceived assumptions, focusing on participants’ narratives.39–43 The absence of personal relationships with participants further minimized undue influence on responses.44,45
Context
The study was conducted within an international tracheostomy community, including patients, caregivers, and healthcare professionals recruited through the Global Tracheostomy Collaborative (GTC) and related community groups.6,46 These settings were selected due to their diverse geographical representation and engagement with tracheostomy care, which provided a broad context for understanding varied experiences across different healthcare systems and support networks.47,48 The international scope of the study allowed the team to capture a wide array of cultural, logistical, and healthcare-related factors relevant to tracheostomy management.49
Sampling Strategy
A purposive sampling strategy was employed to recruit participants who could provide rich, varied insights into the lived experience of tracheostomy care47,50 Inclusion criteria encompassed adults with tracheostomy, caregivers, and healthcare professionals who had first-hand experience with tracheostomy care.51 Participants were recruited via GTC’s email listserv and social media platforms, including Facebook support groups.52,53 Recruitment continued until thematic saturation was achieved, with no new themes emerging.54,55 This sample size and diversity enabled a comprehensive exploration of the topic and enhanced the transferability of findings.56
Ethical Issues Pertaining to Human Subjects
The study received approval from the Institutional Review Board (IRB) and adhered to the ethical guidelines outlined by the University of Michigan’s institutional policy for conducting international surveys (Study eResearch ID HUM00208783).57 All participants were provided with an information sheet detailing the purpose of the study, confidentiality measures, and their right to withdraw.58 Consent was implied through participation in the online survey, which was conducted anonymously to safeguard participant identity.59 Survey data was stored in a secure, password-protected file system accessible only to the research team, ensuring confidentiality and data security throughout the study.60
Data Collection Methods
Data collection involved a cross-sectional survey using open-ended questions, capturing qualitative responses from patients, caregivers, and healthcare professionals involved in tracheostomy care over a period of 6 months. Participants were recruited from the GTC Patient and Family Learning Community, associated Listservs, and tracheostomy-related support groups on social media. This approach allowed us to reach a diverse group across multiple regions and healthcare systems. An iterative process was applied, where responses were reviewed periodically, and the data collection method was refined as needed to capture emerging themes.
Data Collection Instruments and Technologies
Data were collected via an online survey developed and administered using Qualtrics (version 2024, Qualtrics, Provo, UT). The survey included open-ended questions designed to elicit detailed narratives about participants’ experiences, including questions like “What are the primary challenges you face in managing tracheostomy care?” and “What forms of support have been most helpful to you?” Initial testing with a small group of community stakeholders confirmed that these questions were capturing relevant data without needing further modification. No audio or video recording was involved, as responses were submitted as written text directly into the online platform, which facilitated data collection across different time zones and ensured participant privacy.
Units of Study
The study aimed to capture diverse perspectives by including individuals directly involved in tracheostomy care, such as patients, caregivers, and healthcare professionals. Eligible participants were adults with personal or professional experience in tracheostomy care, recruited through the GTC and related community groups. This sampling approach was designed to provide insight into a range of lived experiences within various healthcare settings and cultural contexts, capturing both patient and provider perspectives on the complexities of tracheostomy management.
Data Processing
After survey responses were collected, data were downloaded from Qualtrics in a de-identified format to ensure participant anonymity. Data were securely stored in a password-protected file system accessible only to the research team. The text responses were reviewed and prepared for analysis through a coding process managed in NVivo 12 software. Prior to coding, each response was anonymized, and any identifying details were removed or generalized. This study adhered to established qualitative reporting standards to enhance the transparency and rigor of the research process.61 An audit trail was maintained throughout data processing, documenting data handling and coding decisions to verify the integrity and consistency of the dataset.
Data Analysis
Demographic data underwent descriptive analysis. Thematic analysis was conducted using a six-phase approach as outlined by Braun and Clarke (2006). Two researchers, both experienced in qualitative methods, independently conducted initial coding, identifying significant statements related to participants’ lived experiences with tracheostomy care. Codes were reviewed, compared, and iteratively refined through discussions with the research team, ensuring consensus on the identified themes. This process involved a series of interpretive steps, moving from coding to theme development, and each theme was cross-verified with raw data to maintain fidelity to participants’ narratives. Triangulation with feedback from other researchers familiar with tracheostomy care strengthened the robustness of the findings, while regular reflexive discussions among the researchers minimized potential bias.
Techniques to enhance trustworthiness
To enhance trustworthiness and credibility, the study employed several techniques. An audit trail documented each stage of data collection and analysis to ensure transparency and traceability of analytic decisions. Triangulation involved multiple researchers in independent coding and theme refinement, minimizing bias and validating findings. While member checking was not possible due to survey anonymity, peer debriefing with colleagues experienced in qualitative methods and tracheostomy care provided diverse perspectives and confirmed theme alignment. Reflexive journaling further helped researchers manage assumptions, supporting a balanced and credible interpretation of participants’ lived experiences. Standards for Reporting Qualitative Research was used to report findings.61
Results
Demographics and Participant Characteristics
The study included 191 participants involved in tracheostomy care, representing diverse roles: tracheostomy patients (n = 81; 42.4%), healthcare professionals (n = 63; 33.0%), family members (n = 34; 17.8%), caregivers (n = 9; 4.7%), and healthcare workers with tracheostomy (n = 4; 2.1%). The average age was 48.5 years (SD = 13.2), ranging from 5 to 78. Participants were geographically dispersed across 17 countries, predominantly from the United States (n = 101; 52.9%) and the United Kingdom (n = 33; 17.3%), with additional representation from Australia and Finland (n = 14 each; 7.3%), Canada (n = 7; 3.7%), Brazil (n = 3; 1.6%), Ireland (n = 5; 2.6%), Saudi Arabia (n = 3; 1.6%), and several other countries. Participants resided in urban (n = 90; 47.1%), suburban (n = 67; 35.1%) or rural (n = 34; 17.8%) locations.
Themes
Analysis of participants’ experiences revealed three primary themes: 1) tracheostomy as both a lifeline and a vulnerability, 2) dual-sided risk perceptions, and 3) disrupted care and team function. These themes emphasize the emotional, social, and healthcare challenges encountered by patients, caregivers, and healthcare professionals (Table 1).
Theme 1: Tracheostomy as Both a Lifeline and a Vulnerability
While tracheostomy was viewed as an essential, life-saving intervention, it also emerged as a source of vulnerability. Patients and family members described the tracheostomy as isolating, often “covering up the trach” and “staying inside,” actions that contributed to feelings of social withdrawal and depression. One patient expressed this experience as “having no voice,” emphasizing the communication barriers posed by the tracheostomy. The sense of isolation was further complicated by social stigma, with participants reporting feeling “stared at more than usual” and “treated differently” due to age and health conditions. Additionally, patients and families expressed concerns over being deprioritized in healthcare, fearing that “supplies for home tracheostomy have become the ‘hot item’ for ICUs” and voicing anxiety that “home backup ventilators [might] be taken for use in hospitals.” Participants described exchanging scarce supplies via social media when they could not purchase them. Healthcare professionals echoed this vulnerability, describing patients’ isolation as “a fear of going anywhere.”
Theme 2: Dual-Sided Risk Perceptions
Tracheostomy was perceived as a source of both increased susceptibility and transmission risk. Patients and caregivers expressed fears of contracting infections, with one family member stating, “I am afraid that a nurse, assistant, or physiotherapist will infect me.” Family members similarly worried that interactions with healthcare staff could expose their loved ones to risk. One family member shared, “I fear it is easier for my child to contract the virus because of the trach.” Conversely, participants noted that tracheostomy was perceived by others as a transmission risk, explaining, “Medical professionals are afraid of an open airway.” Another participant observed, “people look at me like I’m a danger to them.” One health professional stated, “Nurses [are] afraid and hesitant to handle patients with tracheostomy.” Another participant described the challenge of maintaining safe practices as “making sure my patients and family members are safe.” Some patients and caregivers noted lack of acknowledgment for the expertise they and their families have developed in managing their own care or that of their loved ones, including innovative solutions to daily challenges.
Theme 3: Disrupted Care and Team Function
Participants reported shortages of supplies, team staffing, and limitations in care delivery. One participant remarked, “It is difficult getting supplies not provided by my DME provider, like gloves and peroxide.” The absence of regular care teams added to patients’ anxiety, with one caregiver sharing, “I was afraid that we were on our own and that the hospital was just open for emergencies.” The pandemic experience left deep emotional marks for many respondents. For example some participants noted that, “Crisis Standard of Care may deprioritize treatment” and limit access to routine evaluations and support. In extreme cases, this translated into a “worry of being left behind” if healthcare needs of all could not be address. Healthcare professionals described worforces constraints. Chronic shortfalls in trained staff and tracheostomy supplies have been recurring challeges. One participant explained that “it is difficult not being able to see my patients in person,” while another noted shortages of medical grade silicone and the challenge of “getting longer use out of equipment,” such as reducing tracheostomy tube changes.
Synthesis and Model Development
Together, these themes reflect a model of compounded vulnerability in tracheostomy care, illustrating how physical, social, and systemic factors interact to shape participants’ experiences. The ICF framework reinforces this interpretation, accounting for the complex interplay between individuals’ health conditions, personal factors, and environmental challenges. The findings underscore the need for a patient-centered approach that considers not only physical needs but also psychosocial and structural factors, for inclusive and adaptive care healthcare models that also aim to maximise individual activities and participation.
Discussion
The themes surrounding tracheostomy care capture the inherent tensions and dualities experienced by individuals with a tracheostomy and those who care for them. Tracheostomy is a lifesaving device that simultaneously creates vulnerability and stigma; it facilitates recovery and independence while introducing risks, and it can serve as a unifying focus for team efforts or highlight the fragmentation of the healthcare system. These complexities reflect not only the physical and medical realities of tracheostomy but also its psychosocial dimensions, which are shaped by the interplay between personal experiences and systemic factors. This study extends existing scholarship by emphasizing how tracheostomy care intersects with themes of isolation, communication barriers, resource shortages, and the heightened challenges during healthcare crises. By situating the findings within prior work, this discussion underscores how tracheostomy care demands an integrated, multidisciplinary approach to address needs of patients
Integration with Prior Work
Prior research has documented how the isolation and communication barriers faced by individuals with tracheostomy can lead to psychological distress and a diminished quality of life.16,17,62 This study corroborates these findings, with participants describing feelings of loneliness, a reliance on social media for communication, and stigma from others. Furthermore, the study highlights how supply shortages, fragmented care, and crisis care policies can exacerbated patients’ fears of being deprioritized or receiving unjust resource allocation. Discomfort with tracheostomy care is common and there is a need for greater emergency readiness.63,64 The concept of tracheostomy as both a lifeline and vulnerability adds depth to prior studies,65,66 which examined communication barriers in tracheostomy patients. Our study shows that these barriers are pervasive and intensified under circumstances of healthcare resource limitations. Additionally, this study supports the call for multidisciplinary approaches in tracheostomy care.
Implications
The findings emphasize the need for tracheostomy care to integrate both physical and emotional support, addressing personal and systemic stresses that disproportionately impact individuals with long-term airway needs. Policies ensuring access to supplies, communication aids, and psychosocial support can help reduce vulnerabilities for patients and caregivers. Additionally, stigma reduction in community and healthcare settings is crucial. Training healthcare professionals to recognize the dual-sided risks faced by tracheostomy patients can alleviate stigmatization, foster trust, and create safer, more supportive environments, ultimately improving overall healthcare experience and long-term outcomes. Ensuring continuity of care, advocating for optimal resource allocation, and incorporating patient and caregiver perspectives into policies can enhance quality of life and societal participation for tracheostomy patients.
Transferability
The challenges identified reflect ongoing issues faced by individuals with tracheostomy worldwide. The study’s diverse sample, spanning multiple countries and healthcare contexts, supports the transferability of these findings. For example, the findings on supply shortages and staffing challenges, as documented in other studies resonate in both high-resource and low-resource settings.20,67 Proactive solutions to resource allocation and interprofessional training could benefit tracheostomy patients globally.
Contributions to the Field
This study underscores the compounded vulnerability of tracheostomy patients, an underexplored concept in the literature.68 By emphasizing psychosocial dimensions, it advocates for holistic, patient-centered approaches to tracheostomy management, expanding interprofessional care.11,22 The findings highlight the critical role of families and care partners in sharing emotional and logistical burdens, aligning with prior work emphasizing caregiver support to improve outcomes26 and fostering sustainable care models through multidisciplinary support.24 Additionally, the study reveals gaps in healthcare infrastructure, as crises exacerbate vulnerabilities in care teams and supply chains, particularly for complex care populations.69,70 By addressing these challenges, this research contributes to healthcare resilience and promotes inclusive, interprofessional, and patient-centered care to enhance quality of life for individuals with tracheostomy.
Limitations
This study provides valuable insights into the lived experiences of individuals with tracheostomies, though limitations in credibility, dependability, confirmability, and contextual strains affect interpretation. The reliance on self-reported survey data limits credibility compared to in-depth interviews, which future studies could address by using semi-structured interviews for richer data. Dependability may be impacted by recruitment through the GTC, which could introduce selection bias, as participants may have had more resources and support than others. While reflexive journaling and peer debriefing were employed to enhance confirmability, achieving complete neutrality is challenging, and anonymity precluded member checking. Contextual strains, such as variations in respondent characteristics and timing, further limit generalizability. Despite these constraints, the study incorporates robust strategies to enhance trustworthiness, including an audit trail and reflexivity, and future research could benefit from broader sampling and longitudinal designs to capture evolving experiences.
Conclusion
This study examines the compounded vulnerabilities, social isolation, and disruptions associated with tracheostomy care. Otolaryngologists, nurses, and allied health professionals are positioned to address these needs as leaders in airway management, communication, and tracheotomy care. The findings call for resilient, patient-centered approaches that reduce stigma and improve societal participation, areas where tracheostomy care teams can lead by fostering multidisciplinary collaboration and education. Future research and leadership in tracheostomy care should aim to build more adaptive and inclusive practices to improve outcomes and equitable care.
Disclaimer
The information or content and conclusions do not necessarily represent the official position or policy of, nor should any official endorsement be inferred by the Department of the Army, Department of Defense, or U.S. Government.
Funding
Research reported in this publication was supported by the Agency for Healthcare Research and Quality (AHRQ) of the U.S. Department of Health and Human Services under Award Number R18HS029124. Dr. Vinciya Pandian is the Contact Principal Investigator for this project, conducted through the Center for Immersive Learning and Digital Innovation: A Patient Safety Learning Lab. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality or the U.S. Department of Health and Human Services.