Tracheostomy is a life-sustaining intervention for individuals with a wide array of complex medical needs. Within the tracheostomy community are newborn infants first opening their eyes to the world, elderly adults in the twilight of their life journey, and every possible stage between, whether navigating congenital conditions, airway obstruction after trauma, or recovering from neurologic injury, or prolonged mechanical ventilation. Yet patients with tracheostomies are frequently invisible in policy discussions, despite their reliance on the pillars of academic medicine and public insurance. The advances of recent decades in care illustrate what is possible when teams, research infrastructure, and coordinated policies work in unison. Sustained investment in academic research and Medicaid coverage thus represents moral imperatives to achieve better, safer, equitable care.
A Fragile Lifeline
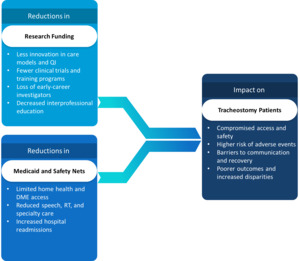
Many of the systems that support the tracheostomy community are linked to federally funded research and public insurance. Recent proposals to reduce NIH-funded research, along with cuts to Medicaid, risk dismantling the very infrastructure that has made innovation in tracheostomy care possible. These changes are not abstract budgetary maneuvers; they would directly compromise the care of individuals who depend on coordinated, multidisciplinary, and evidence-based approaches. From premature infants requiring airway support in neonatal intensive care units to adults with neurologic injury needing long-term ventilation and communication assistance, this population represents those for whom disruption in services could be life-altering or even life-threatening.
The fragility of this ecosystem lies in its dependence on sustained, synergistic investment. Academic research institutions generate the knowledge and tools that shape best practices, while Medicaid ensures access to these practices for patients who often have no alternative means of coverage. Undermining either pillar destabilizes the system and the lives it supports. Loss of Medicaid reimbursement could mean fewer home health visits, less duty care nursing, reduced access to speaking valves and supplies, and institutional reluctance to accept high-risk transfers. At the same time, a weakened academic research infrastructure curtails clinical trials, workforce development, and the dissemination of innovations that improve safety and quality of life. These parallel threats must be understood not only as financial decisions but as choices with ethical consequences.
Academic Medicine as an Engine for Tracheostomy Innovation
Over the past decade, a growing body of literature has highlighted the role of academic medicine in transforming tracheostomy care. Multidisciplinary collaboratives such as the Global Tracheostomy Collaborative (GTC) have harnessed the power of data registries, structured education, and standardization to reduce morbidity, improve communication, and shorten hospital stays.1,2 Academic-led initiatives like the “Trach Trail” have demonstrated how interprofessional pathways rooted in quality improvement science can streamline transitions from ICU to home and reduce adverse events.3
The success of these efforts has been investigated at scale with demonstration projects across large numbers of community and academic hospitals.4 Innovation also occurs in educational innovation and new strategies to improving care.5 Such progress, however, depends on academic ecosystems that support interprofessional teams, simulation training, and translational research. Systematic reviews confirm that interprofessional tracheostomy teams improve outcomes across multiple domains: earlier speaking valve use, faster time to speech and decannulation, and reduced complications.6 These benefits are not hypothetical; they are reproducible, scalable, and measurable.
The Return on Research Investment
The economic rationale for research investment is compelling and well-documented. For every $1 the NIH invests, the return to the U.S. economy is estimated at $2.46, emphasizing the value of research not only in scientific advancement but in national economic vitality.7 In tracheostomy care specifically, the dividends of this investment are tangible and far-reaching. Federally funded projects have supported centers for immersive technology and digital innovation as well as multicenter trials that inform evidence-based practice. In the US and abroad, investment has enabled the development of tools that enhance safety at the bedside and facilitated the creation of care pathways that reduce variability and standardize best practices.3,8–10 These investments have contributed to measurable improvements in patient outcomes and health system efficiency.
The most important metric on return on research is not financial but human. Patients gain access to communication through earlier one-way speaking valve use, timelier decannulation, and fewer complications. Families gain clarity, hope, and support during vulnerable moments of their lives. Providers benefit from evidence-informed guidance that reduces uncertainty and improves confidence in care delivery. Institutions, in turn, gain frameworks for scalable innovation that can be adopted across diverse care settings.4,11 These investments proved critical in navigating the unique challenges of patients with tracheostomy in the pandemic era and beyond.12–18 The transformative achievements of the past 25 years are rooted in the sustained support of academic research infrastructure. Without it, the momentum slows, and the patients are the first to feel its absence.
Medicaid and the Safety Net for Tracheostomy Patients
Medicaid is the largest source of health insurance for medically complex and low-income individuals in the United States. It provides coverage to more than 72 million Americans, including 40% of all children, 63% of nursing home residents, and nearly half of children with special healthcare needs.19,20 Its role is critical for people who fall outside the reach of employer-sponsored insurance or Medicare, which includes those living with chronic disability, unstable employment, or caregiving burdens, all of which can occur with tracheostomy. Patients with tracheostomies are disproportionately represented in these categories, whether due to neurologic or genetic conditions, traumatic brain injury, spinal cord trauma, or prolonged intensive care unit (ICU) stays with complex rehabilitative care.
For these individuals, Medicaid is not a supplemental payer or a secondary option; instead, it is often the sole lifeline to ongoing treatment, durable medical equipment, home nursing, and specialty follow-up (Table 1).21–23 It covers speech-language pathologists who enable communication and optimize swallowing function, respiratory therapists who manage ventilator settings, and home health aides and nurses who assist with daily living. In rural and underserved areas, where provider shortages are common and private insurance options limited, Medicaid is often the only viable pathway to receive the multidisciplinary, coordinated care that tracheostomy patients require to survive and thrive.19 Without it, access to essential services collapses, and patients may face avoidable hospitalizations, prolonged institutionalization, threats to safety, or deterioration in quality of life.
What is at Risk?
Congressional proposals to cut Medicaid by over $880 billion over ten years threaten to destabilize care for millions19,20 As illustrated in Figure 1, simultaneous reductions in Medicaid and federally funded research have compounding effects—limiting access to home care, stalling clinical innovation, and ultimately placing tracheostomy patients at heightened risk. If enacted, these cuts would force states to reduce eligibility, restrict services, and lower already modest provider reimbursement rates.20 For tracheostomy patients, this could translate into reduced access to home nursing, fewer options for specialty follow-up, and higher rates of preventable complications.
Work requirements and other administrative procedures proposed in the Make America Healthy Again executive order could have significant implications for coverage.20 For example, clinicians may be asked to determine whether a patient is “disabled enough” to qualify for care, placing clinicians in ethically fraught positions with the needs and well-being of their patients in the balance. The implications for patients with often misunderstood conditions like tracheostomy could range from missed visits to delayed interventions, or denial of life-sustaining supplies.
Threats to the Academic Ecosystem: NIH Cost Cuts
Proposed reductions in federal grant and research investment could have far-reaching implications (Table 2). These changes range from the portfolio of research projects supported to the merging or dissolution of whole institutes such as the Agency for Healthcare Research and Quality. Proposals to reduce indirect cost rates on grants represent a quieter but equally ominous threat to the infrastructure supporting tracheostomy research. These funds are used to maintain labs, equipment, compliance offices, and research administration. As a result, they are the scaffolding upon which innovation depends. A reduction in rates from ~50% to 15% would severely limit the capacity of research-intensive institutions to sustain operations.7
As Sandro Galea and colleagues warn in JAMA, such abrupt changes pose “an existential threat to academic health research”.7 These indirect costs enable the multicenter, multidisciplinary initiatives that have transformed tracheostomy care. Without them, much research grinds to a halt. As early-career investigators leave, research infrastructure lays fallow and a next generation of clinician-investigators never gains footing. The downstream implications for patient care will become increasingly apparent in years to come.
From Policy to Patient: Why Investment in Research and Medicaid Matters
In the case of the improvements tracked by the GTC across participating hospitals, it took years to build the database infrastructure, forge relationships, and implement demonstration projects. Data-driven protocols led to faster decannulation, improved one-way speaking valve access, and fewer ICU days.4,6 Similarly, pediatric models at academic children’s hospitals have improved discharge planning and decreased readmissions.3,8 While highly cost-effective these are not low-cost interventions. They require nurse educators, simulation labs, care coordinators, and data analysts. Effective care requires Medicaid to reimburse home ventilator care and academic health systems to subsidize care coordination. Cut either link in the chain, and the system falters.
In this sense, academic research and Medicaid are co-dependent systems: the former develops the models, the latter implements them in the real world. Without Medicaid, even the most rigorously tested, evidence-based interventions remain out of reach for the patients who need them most; without research, there is no roadmap to guide safe, effective, and equitable care delivery. The tracheostomy community exemplifies this interdependence. Academic institutions generate care pathways that integrate respiratory therapy, speech-language services, and caregiver education, and Medicaid makes these pathways actionable by funding home nursing, durable medical equipment, and rehabilitative services. Disrupting either component disrupts the fragile ecosystem; sustained alignment is needed to advance care for patients with complex needs.
Moral and Economic Imperatives3,8
Patients with tracheostomies need the best care science can offer. To ask clinicians to enforce Medicaid work requirements or to ration essential services due to budgetary pressures is medically unsound and ethically problematic.19,20 Such mandates risk eroding the trust between patients and providers by placing clinicians in roles that conflict with their core duty to advocate for patient welfare. Policy changes policies have far-reaching societal implications. Barriers to care can be compounded by systemic bias, language discordance, lower health literacy, and geographic inequity. Disinvesting in the public insurance, academic health centers, and community-based services can perpetuate health disparities. Upholding public safety nets and supporting academic research are not only sound economic choices but also moral imperatives grounded in a commitment to compassion and trust.
Conclusion
The science of tracheostomy care is emblematic of what public investment in research and patient care can achieve. Defunding research and Medicaid risk severing critical lifelines for patients, families, and those who dedicate their lives to supporting them. Without these supports, lives become precarious, and hard-won gains can begin to unravel. Research in progress has already improved the odds for thousands of patients with tracheostomies. Sustaining that progress requires vigilance, vision, and political will. Investing in science and safety is a choice to sustain progress by breathing life into our shared mission of improving the lives of every individual with a tracheostomy.