Introduction
Proficiency in comprehensive tracheostomy care is critical for preventing and managing airway emergencies, as well as avoiding chronic complications such as stomal breakdown, airway stenosis, and respiratory infections. However, tracheostomy care is complex, labor intensive, and can be required for patients with a wide array of medical conditions, often involving a need for prolonged mechanical ventilation or chronic respiratory care.1,2 Disparities in provider training, patient education, and healthcare accessibility continue to adversely affect clinical outcomes.3,4 Recognizing the transformative potential of artificial intelligence but also the need for guardrails, several guiding principles have been proposed, focusing on the collaborative role of technology and need for transparency and oversight in reporting and implementation.5–8
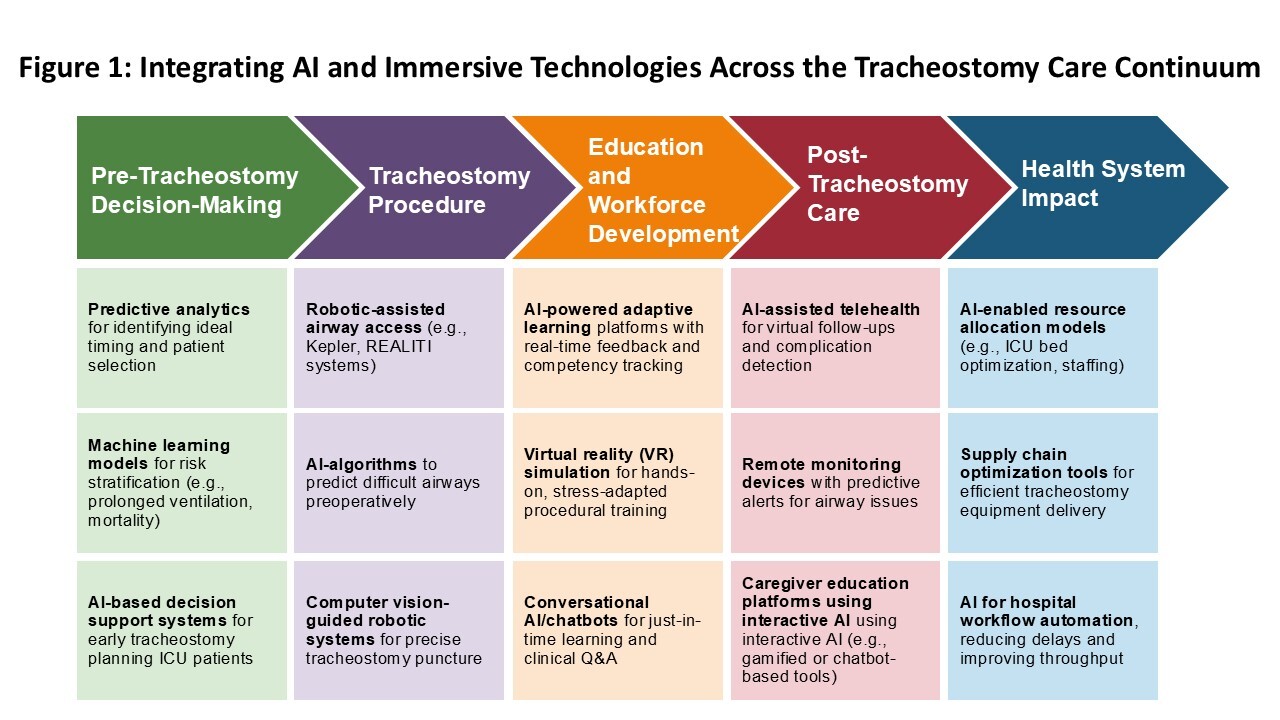
Previous studies have highlighted gaps in knowledge that impede clinical decision making. For example, it is challenging to anticipate the necessary duration of mechanical ventilation,9 an area where predictive analytics would be valuable. There is also a need for artificial intelligence (AI)-based decision support in tracheostomy placement10 and digital health tools for improving patient self-management.11,12 AI and digital health solutions offer the promise of bridging these gaps by enhancing education, optimizing clinical decision-making, and ensuring cost-effective care delivery. However, challenges remain in assuring the safety and reliability of such tools, achieving transparency in algorithms, and mitigating the risk of bias. This article explores the current state and near-term prospects for integrating AI-driven technologies and simulation in areas of tracheostomy education, telehealth, predictive analytics, and robotic-assisted airway management. To illustrate the multifaceted role of artificial intelligence and immersive technologies across the stages of tracheostomy care, Figure 1 presents a conceptual continuum. This schematic maps how emerging innovations—from predictive analytics and robotic assistance to virtual training, telehealth, and system-level optimization—are redefining airway care delivery across inpatient, outpatient, and virtual domains.
AI-Driven Tracheostomy Education and Workforce Development
Effective tracheostomy management requires a high level of clinical expertise, yet persistent knowledge and skill gaps among healthcare providers contribute to inconsistent care, increased complications, and patient safety risks, as evidenced by the global needs assessment in this issue. Traditional training models, such as didactic lectures and hands-on workshops, often fail to provide individualized learning experiences, leaving clinicians underprepared for critical scenarios. Moreover, the complexity of tracheostomy care demands a nuanced understanding of airway management, interdisciplinary coordination, and emergency response protocols. The variability in institutional protocols exacerbates these challenges, leading to inconsistencies in care delivery and outcomes. Without structured, competency-based learning models, healthcare providers may struggle to maintain proficiency in low-frequency, high-risk tracheostomy scenarios, ultimately compromising patient safety.
Several studies have highlighted subjective discomfort and demonstrable deficits in tracheostomy-related competencies, particularly in emergency management and distinguishing between tracheostomy and laryngectomy. For example, one study by Morris et al. reported that while 70.9% of nurses felt confident in suctioning and 58.2% in stoma care, only 18.2% were confident in managing tracheostomy emergencies, and a mere 10.9% could differentiate between a tracheostomy and a laryngectomy.13 Over half of US otolaryngologists responding to a national survey reported witnessing attempted oral intubations in laryngectomy patients, with a 26% mortality rate.14 Khanum et al. found that tracheostomy knowledge levels ranged from 48% to 52%, corresponding to limited understanding.15 These knowledge gaps correlate with preventable complications such as infection, airway obstruction, and tube dislodgement, contributing to increased morbidity and mortality. Addressing these gaps requires scalable training solutions that enhance theoretical knowledge and procedural confidence.
AI-driven education incorporating machine learning and other digital technology can personalize learning, optimize skill acquisition, and enhance clinical decision-making. AI-powered platforms provide adaptive training experiences, real-time feedback, and competency tracking to ensure clinicians develop proficiency in critical tracheostomy care areas. AI-enhanced modules have been shown to significantly improve procedural accuracy and reduce errors. Studies have shown that AI-driven training improved procedural accuracy by 30%, and reduced critical errors related to tracheostomy management by 40%.16,17 Moreover, AI-based educational tools can enhance overall clinical management by improving mechanical ventilation management, pulmonary diagnostics, and remote patient monitoring. Karthika and colleagues demonstrated that AI-assisted patient monitoring improved early complication detection rates by 25%, allowing for timely intervention and reduced adverse outcomes.18 These findings highlight the capacity of AI to address competency gaps and reduce dependence on more resource-intensive traditional training models.
In addition to structured AI-driven training programs, applications involving conversational AI—such as chatbots and virtual assistants—can offer real-time clinical decision support, self-directed learning, and knowledge reinforcement. In some studies, AI chatbots demonstrate superior accuracy in tracheostomy-related inquiries compared to human clinicians. A cross-sectional study found that ChatGPT-4.0 achieved 64.3% accuracy in answering tracheostomy care-related questions, significantly outperforming clinical nurses (36.7%).19 These AI systems excelled providing guidance on airway humidification, suction techniques, and complication management; however, the effectiveness of AI-based virtual assistants relies on engagement, trust-building, and empathetic communication. A review of 48 studies found that AI chatbots with realistic medical avatars increased learner engagement by 50% compared to traditional text-based interfaces.20 AI chatbots could mitigate accessibility challenges by providing scalable and cost-effective remote education, addressing a pressing need in resource-limited environments.21
Despite these advantages, AI-driven education also has limitations. While AI-generated tracheostomy care recommendations have demonstrated high factual accuracy, concerns remain regarding readability, complexity, and the potential for misinformation. A cross-sectional study found that ChatGPT responses scored an average of 3.55/5 for factual accuracy and 4.02/5 for overall quality.22 Furthermore, the readability of AI-generated content was problematic, with an average Flesch-Kincaid Grade Level of 13.1 (SD = 1.47), far exceeding the National Institute of Health-recommended sixth-grade level for patient education materials,22 although AI is can simplify reading level when so instructed. These observations highlight the adjustments needed to improve readability and ensure appropriate contextualization for patient-facing applications. Moreover, AI-generated responses occasionally included misleading or incomplete information, emphasizing the need for human oversight and further refinement of AI algorithms to enhance specificity and reliability.
The integration of AI into tracheostomy education offers a paradigm shift in workforce development, offering interactive, scalable, and personalized learning solutions that address critical competency gaps. AI-driven platforms not only enhance skill acquisition and clinical confidence but also expand access to expert knowledge, optimize learning outcomes, and improve patient safety. As AI technology continues to evolve, future research should focus on refining algorithm transparency, improving content readability, and balancing AI automation with human expertise to maximize its effectiveness in clinical education and patient care. A summary of the most impactful AI-driven innovations in tracheostomy care—including applications in education, simulation, telehealth, predictive analytics, and robotics—is presented in Table 1. These examples demonstrate how AI technologies are reshaping care delivery across the tracheostomy continuum.
Digital Simulation and Stress Adaptation in Tracheostomy Training
Virtual reality (VR) is modernizing healthcare education by providing immersive, controlled environments that enhance learning and reduce stress. AI-generated VR fosters engagement while mitigating anxiety, making it a promising tool for clinical training. Stress can impede learning in clinical settings.23–27 Meese et al. (2021) highlight VR’s potential to reduce stress-related challenges, enhance performance, and improve emotional well-being.28 Elendu et al. (2024) support these findings, emphasizing that VR simulation allows repeated practice of complex procedures without real-patient risks, reducing performance anxiety and improving decision-making and teamwork.29 Liaw et al. (2022) found that VR induces similar physiological stress responses as face-to-face (F2F) simulation, yet learners maintained comparable performance and confidence.30 The negative correlation between stress and confidence (r = −0.43; p < 0.01) suggests that VR fosters resilience and improves stress management over time.30
Tracheostomy care requires precision and confidence. Abbas et al. evaluated a VR training tool for pediatric emergency tracheostomy skills, engaging 69 professionals in an immersive, remote-access training program.31 Findings suggest VR training is as effective as traditional mannequin-based methods.16 Abbas also compared VR-based tracheostomy safety training to F2F instruction, showing that while both groups improved knowledge (F2F: +2 points; VR: +4 points, p = 0.21), VR learners started with lower baseline scores but demonstrated high usability and comfort.31 Despite taking longer in emergency scenarios (194.3 vs. 137.4 seconds, p = 0.002), participants rated VR training positively for accessibility and effectiveness.31 Chiang et al. demonstrated that VR training significantly improved healthcare providers’ and patient families’ confidence (92% vs. 74%, p = .001) and reduced anxiety (93% vs. 75%, p = .002) compared to traditional text-based methods.17 Training benefits were sustained for up to four weeks post-intervention.17 Bayram and Caliskan examined a game-based VR app for tracheostomy care, revealing significantly higher test scores in suctioning (p = 0.017) and peristomal skin care (p = 0.003) among VR learners, supporting its integration into nursing curricula.32 In tracheostomy care, VR training can build confidence, improve retention, and offer scalable learning. Further research is needed to optimize VR’s implementation and assess associated clinical education and patient care outcomes.
AI-Enabled Telehealth for Tracheostomy Follow-Up Care
Providing follow-up care for individuals with a tracheostomy in the community is challenging due to complex medical needs, caregiver burden, and limited access to specialized providers. An article in this issue highlights how barriers such as long travel distances, financial constraints, and inadequate tracheostomy training contribute to delayed interventions and increased hospitalizations. Telehealth, particularly AI-driven applications allows for remote monitoring, early complication detection, and real-time caregiver support.33 AI algorithms can analyze patient data, generate alerts, and facilitate virtual interactions, optimizing care delivery and reducing unnecessary healthcare utilization.34
Two recent studies have explored telehealth for tracheostomy care. Gözetici and Dönmez evaluated a six-week digital education–supported telehealth program for mothers of children with tracheostomies, finding no significant change in hospital admissions (p = 0.079) or complication rates (p = 0.286), but an improvement in tracheostomy care knowledge (p < 0.001) and a decreasing trend in caregiver burden (p = 0.058).12 Similarly, Moreno and Peck implemented a nurse practitioner-led telehealth initiative in South Texas, replacing a four-week in-person visit with a virtual follow-up at two weeks post-discharge. Although limited by a small sample (n=2), caregivers reported improved knowledge and self-efficacy, with no complications, emergency visits, or hospitalizations within 30 days.35
There has also been significant interest in the potential of telehealth to improve tracheostomy care in the pediatric population. A study by Tovichien et al. demonstrated that a telehealth program incorporating respiratory care training and family support significantly reduced hospital readmission days, admission costs, and ICU admission rates for children with tracheostomies. Specifically, the median number of admission days decreased from 55 to 6 days, and ICU admission rates dropped from 43.8% to 2.1% (p < 0.001). Additionally, caregivers’ confidence in managing tracheostomy care increased from 47.9% to 85.5% immediately after the program.36 Gözetici and Dönmez’s study on digital education-supported telehealth interventions for mothers of children with tracheostomies found that such programs significantly increased the mothers’ knowledge levels about tracheostomy care (p < 0.001) and reduced their care burden, although there was no significant change in the number of complications or hospital admissions.37
Broader research supports telehealth’s effectiveness in improving access and outcomes. A scoping review by Choi et al. highlights AI-assisted telehealth’s role in enhancing user satisfaction, diagnostic accuracy, and remote patient monitoring.34 Bowman et al. discuss telehealth’s expanding role in primary care post-COVID-19, emphasizing AI-driven decision support and data-driven triage.38 These findings suggest that AI-enhanced telehealth could further optimize tracheostomy management by integrating real-time monitoring, predictive analytics, and caregiver education. At the same time, the opportunity from telehealth can be limited by the digital divide,39 and approaches must ensure access both from the perspectives of connectivity and the skills of patients and clinicians to use the technology.
Future research should validate AI-assisted telehealth models to improve accessibility, reduce hospitalizations, and enhance outcomes for tracheostomy patients.
Evolving Role of Predictive Analytics in Preventing Tracheostomy-Related Complications
Predicting the right patient and optimal timing for tracheostomy remains debated due to varying clinical factors and the lack of standardized guidelines.40–43 Tracheostomy can accelerate liberation from the ventilator, reduce need for sedation, and overall resource capacity strain41; however, there are also potential negative implications, such as eligibility for patients for accessing care, such as the reluctance of rehabilitation centers to accept stroke patients with tracheostomy, which may affect recovery of function during critical windows. Advances in predictive analytics, particularly ML and deep learning, are increasingly supporting decision-making by analyzing large datasets to identify patterns for patient-specific recommendations. These technologies enhance risk stratification, enable early intervention, and optimize healthcare resources, ultimately improving patient outcomes and reducing complications.
Machine Learning for Risk Prediction and Prevention
Hidaka et al. leveraged ML techniques, including random forest and multivariable logistic regression, to predict tracheal necrosis following total pharyngolaryngectomy with free jejunal transfer.44 Their model demonstrated high predictive accuracy (92.7% overall; 95.9% for severe cases), identifying history of radiotherapy (OR = 4.34, p = 0.001), total thyroidectomy (OR = 3.25, p = 0.042), and paratracheal lymph node dissection (OR = 3.42, p = 0.015) as key risk factors.44 The study emphasized the importance of preoperative risk stratification and intraoperative modifications, such as preserving thyroid vascular supply and limiting lymph node dissection, to prevent tracheostomy-related complications.44
Nguyen et al. develop an ML-based predictive model to determine the likelihood of tracheostomy need in mechanically ventilated patients at intensive care unit (ICU) admission.10 Using XGBoost on data from 38,508 patients, their model achieved an AUROC of 0.794, identifying pneumonia, sepsis, and chronic respiratory failure as key predictors.10 These findings reinforce the potential of ML in guiding early tracheostomy decisions and reducing complications associated with prolonged ventilation.10 Abujaber et al. further demonstrated the role of ML in early tracheostomy planning by predicting prolonged mechanical ventilation in traumatic brain injury patients.45 Their support vector machine model achieved high accuracy (0.79) and area under the curve (0.84), with key predictors including ventilator-associated pneumonia, blood transfusion, and Glasgow Coma Score.45 These insights highlight a potential role for predictive models in informing decision on tracheostomy placement and improving clinical outcomes.
AI-Driven Tracheostomy Decision Support Systems
Li et al. developed an AI-based decision support system to predict tracheostomy necessity in burn patients.46 Their XGBoost model, trained on data from 1,011 patients, achieved high predictive accuracy (AUROC >0.95), identifying age, days post-burn, consciousness disturbance, total burn index, local burn index, and inhalation injury as key predictors.46 This system, featuring an AI-based nomogram and online calculator, enhances decision-making in resource-limited settings by providing standardized tracheostomy risk assessments.46 Chen et al. applied deep learning techniques to predict tracheostomy need in deep neck infection patients, achieving 78.66% accuracy.47 Utilizing computed tomography-based predictors such as abscess diameter and tracheal proximity, their model assists clinicians in airway management, particularly those with less experience.47
Prognostic Models for Long-Term Outcomes
George et al. employed deep learning models to predict 3- and 12-month mortality in ICU patients requiring prolonged mechanical ventilation.48 Their neural network model, utilizing 250 clinical variables from the Medical Information Mart for Intensive Care (MIMIC)-III database, outperformed the conventional ProVent model (AUROCs: 0.74 vs. 0.59 for 3-month mortality; 0.76 vs. 0.63 for 12-month mortality).48 Predictive factors included advanced age, Simplified Acute Physiology Score II score, renal replacement therapy, and abnormal heart rate and sodium levels.48 These findings support the integration of ML models into electronic health records to improve prognostic discussions and decision-making regarding tracheostomy placement.
Machine Learning for Pediatric Airway Management
Shim et al. and Zhou et al. applied ML models to optimize pediatric airway management, reducing risks such as hypoxia and pneumothorax.49,50 Shim et al. developed a random forest model predicting optimal tracheal tube insertion depth with 79.0% accuracy, outperforming traditional formula-based methods.49 Zhou et al. validated ML models for pediatric endotracheal tube size selection, with random forest models achieving superior predictive accuracy compared to conventional age-based formulas.50 These studies demonstrate the role of ML in enhancing airway management and preventing tracheostomy-related complications in pediatric populations.
The integration of predictive analytics in tracheostomy care is transforming clinical practice by enabling precise risk assessment, optimizing procedural decisions, and preventing complications. ML and AI-driven models facilitate earlier interventions, reduce prolonged mechanical ventilation risks, and improve patient outcomes. However, prospective validation and multi-center studies are essential to ensure the real-world applicability of these models. As predictive analytics continue to evolve, their incorporation into clinical workflows will enhance patient safety and tracheostomy management.
AI-Assisted Robotics in Airway Management and the Emerging Role in Tracheostomy
Robotic innovations are improving airway management through automated navigation in endotracheal intubation and by enhancing precision, reducing complications, or improving procedural efficiency.51 Khan and Karmakar highlighted several advancements in robotic-assisted intubation, such as the Kepler Intubation System (KIS),52 which demonstrated a 91.7% success rate in human tracheal intubation with a mean intubation time of 93 seconds.53 Similarly, the Remote Robot-Assisted Intubation System (RRAIS) improved first-attempt success rates (80% vs. 40%) compared to direct laryngoscopy, although it required slightly more time (75 vs. 53 seconds, p < 0.01).54 The REALITI system, integrating image-recognition software for automated tracheal access, has further refined robotic-assisted airway management, significantly improving both speed and accuracy.55
AI is also playing an increasing role in airway management, with predictive models being developed to identify difficult airways with high sensitivity (80.5%) and specificity (83.3%).56 Robotic prototypes such as IntuBot, which utilizes vision-based navigation, have demonstrated high accuracy in automating intubation.57 Additionally, robotic-assisted airway support systems have been developed to maintain airway patency during general anesthesia and deep sedation, further broadening the scope of AI-driven airway management.58 While cost, technical complexity, and training requirements remain challenges, these innovations hold significant promise in enhancing procedural outcomes, particularly in high-risk or emergency situations.59
Despite these advancements in robotic-assisted airway management, robotic applications in tracheostomy care remain limited. Xiao et al. conducted a pilot study on a trans-oral robotic-assisted needle direct tracheostomy puncture, exploring an alternative to conventional open tracheostomy and percutaneous tracheostomy in patients requiring prolonged mechanical ventilation.60 Although open tracheostomy offers superior visualization, it carries a higher risk of infection and bleeding.61,62 Conversely, percutaneous tracheostomy, while less invasive, is often limited by imprecise puncture placement, increasing the risk of complications such as cricoid injury, deformation of tracheal rings, and vascular damage.63–65 To address these concerns, Xiao et al. (2021) developed a flexible mini-robotic system utilizing robotic needling technology to perform an “inside-out” puncture, allowing precise tracheal access with controlled force application. Their prototype, incorporating a flexible tube, stabilization balloon, and an optic fiber for enhanced visualization, demonstrated promising results in phantom testing, successfully puncturing porcine cartilage and maintaining stability. However, further validation through cadaver and clinical trials is necessary before widespread adoption.
One of the few AI-integrated robotic tracheostomy simulators currently being explored in this issue is AvTrach, which incorporates robotics to simulate breath sounds and other tactile systems to enhance the procedural experience. This innovation represents a step toward bridging the gap between robotic airway management and tracheostomy, suggesting that the principles successfully applied in robotic intubation could be adapted for safer and more precise tracheostomy techniques. While robotic-assisted airway management continues to advance, its expansion into tracheostomy remains nascent. The need for improved precision, reduced complications, and enhanced safety in tracheostomy procedures presents an opportunity for further research and development of AI-driven robotic solutions tailored for this domain.
Cost-Effective AI Solutions for Tracheostomy Care
AI is also affecting healthcare economics, with potential for improvements in resource allocation, cost reduction, and decision-making, particularly during crises such as pandemics and mass casualty events.66 Traditional hospital management often relies on historical data and intuition, leading to inefficiencies such as ICU bed shortages in some areas while others remain underutilized, resulting in an estimated $750 billion in wasteful healthcare spending annually.67 AI-driven models, including Reinforcement Learning (RL), Genetic Algorithms (GA), and the Traveling Salesman Problem (TSP), offer real-time, data-driven solutions that enhance hospital logistics, ensure equitable resource distribution, and improve cost-effectiveness. During the COVID-19 pandemic, AI-supported telehealth services reduced emergency room visits by 42% and hospital admissions by 33.7%, demonstrating AI’s ability to optimize patient flow and reduce unnecessary hospitalizations.68,69
Another study developed a generic health-economic model to assess the cost-effectiveness of AI systems in the ICU.70 This model can simulate various clinical scenarios and estimate the cost-effectiveness of AI interventions, including those related to tracheostomy care. The model supports decision-making by providing early health technology assessments, which can guide the deployment of AI systems in a cost-effective manner. Additionally, AI has been used to analyze breathing sounds in tracheostomy patients to detect airway problems early. This system can classify breathing sounds with high accuracy, enabling timely interventions such as suctioning or tube replacement, which can prevent complications and reduce healthcare costs.71
AI-driven resource allocation models are beneficial in high-demand areas such as tracheostomy care, where real-time access to ventilators, trained personnel, and post-acute rehabilitation resources is critical. Tracheostomy patients require specialized multidisciplinary care, and inefficiencies in resource distribution can lead to increased hospital readmissions, prolonged ICU stays, and higher mortality rates. Genetic Algorithms-based models optimize hospital readiness by analyzing variables such as hospital ratings, mortality rates, bed capacity, and cost per patient, resulting in a 20% reduction in emergency spending and a more equitable distribution of healthcare resources.72 AI-based decision-support systems can help tracheostomy teams identify the most efficient allocation of skilled personnel, reduce delays in decannulation protocols, and prevent complications such as ventilator-associated pneumonia and central line-associated bloodstream infections), conditions that significantly impact healthcare costs and patient outcomes.
Beyond resource management, AI is transforming tracheostomy supply chain logistics through the TSP algorithm, which optimizes medical equipment distribution and reduces transportation costs. AI-driven logistics models have improved healthcare supply chain efficiency by 68%, ensuring faster delivery of tracheostomy tubes, humidification systems, and speaking valves to hospitals and rehabilitation center.72 These improvements are valuable for rural and under-resourced areas where delayed access to tracheostomy supplies can result in extended ICU stays and increased healthcare costs. Additionally, AI-powered telehealth platforms can enable remote consultations, caregiver education, and early detection of complications, reducing hospital dependency and improving patient quality of life.72
By integrating AI-driven models into tracheostomy care and hospital management, healthcare institutions can achieve cost savings, optimized resource allocation, and improved patient outcomes. The AI-driven RL model –which categorizes hospitals into Idle (sufficient resources) or Share (in need of additional resources)– can help tracheostomy teams anticipate and redistribute resources dynamically.66 As tracheostomy care continues to expand beyond critical care settings, AI-powered systems will play an essential role in streamlining workflows, reducing costs, and enhancing patient-centered care. By leveraging AI, hospitals and healthcare policymakers can create a more efficient, equitable, and cost-effective model for tracheostomy management, ensuring that every patient receives the right care at the right time, while minimizing healthcare waste and improving overall economic efficiency.
Conclusion
As AI and immersive technologies continue to expand in clinical practice, it is critical to address persistent challenges to ensure safe, equitable, and effective implementation. Table 2 outlines these challenges and proposes solutions related to algorithm transparency, content readability, workflow integration, and cost-effectiveness. The integration of AI-driven technologies is transforming tracheostomy education, clinical practice, and healthcare logistics, offering scalable and personalized solutions to longstanding challenges in airway management. AI-powered adaptive learning, virtual simulations, and conversational AI have the potential to close knowledge gaps, improve skill acquisition, and enhance clinical decision-making. Moreover, AI-enabled telehealth, predictive analytics, and robotic-assisted procedures are poised to optimize procedural planning, reduce complications, and alleviate provider workload. However, ensuring algorithmic transparency, improving content readability, and maintaining human oversight remain essential to maximizing AI’s benefits while mitigating risks. Future research should focus on refining AI models, validating clinical effectiveness, and integrating these innovations into standardized care pathways. By harnessing the power of AI, healthcare systems can enhance tracheostomy education, improve patient safety, and create a more efficient, equitable, and cost-effective model of care.
Funding & Disclosures
Funding: Center for Immersive Learning and Digital Innovation (AHRQ R18 - HS029124, PI Vinciya Pandian)
Disclosures
None