Introduction
Tracheostomy care is essential for ensuring patient safety and preventing critical complications such as airway obstruction, hemorrhage, and accidental dislodgment.1–4 Proper management of airway secretions through effective suctioning techniques is fundamental to tracheostomy care. Suctioning maintains airway patency, supports pulmonary hygiene, protects surrounding skin, and reduces aspiration risk. Competency in suctioning is also crucial for addressing tracheostomy-related complications, including bleeding, stoma site breakdown, pressure injuries, and device occlusion.5–7 Nurses play a key role in tracheostomy care by performing suctioning, stoma care, and tube changes, and educating patients on evidence-based practices. Other professionals, including respiratory therapists, speech-language pathologists, and physical therapists are integral to post-tracheostomy rehabilitation, highlighting the importance of interprofessional collaboration.
The ability to manage emergencies involving tracheostomies requires technical expertise and the capacity for prompt decision-making. However, novice healthcare professionals often face challenges in tracheostomy care due to limited clinical exposure and reliance on foundational knowledge, leading to heightened anxiety or discomfort. Conversely, experienced professionals leverage substantial practice and critical decision-making skills but may still express apprehension when managing complex tracheostomy situations.8 Inadequate or inconsistent training during academic preparation and in clinical settings further exacerbate these challenges.8–11
Clinical exposure to tracheostomy care is often sporadic, with patients dispersed throughout the hospitals, reducing opportunities for healthcare professionals to develop confidence and mastery.10 Physical fidelity, or the extent to which simulation tools replicate anatomical and procedural elements, is critical in addressing these gaps. Equally important is conceptual fidelity, which ensures the training environment provides cues and contexts that reflect real-world clinical scenarios. Psychological fidelity, emphasizing emotional and cognitive engagement, is essential for fostering learner immersion and preparing healthcare professionals to manage high-pressure situations effectively.12 Together, these dimensions of fidelity underpin the effectiveness of simulation-based training, making it an indispensable component of healthcare education. By integrating hands-on training into academic programs, healthcare professionals can build competency and confidence to manage routine care and respond effectively during emergencies, such as hemorrhage, obstruction, or accidental dislodgment.
Background
Historically, tracheostomy education has relied heavily on real-time experiences. However, these opportunities often lack sufficient supervision and structured practice, increasing the risk of adopting improper techniques.10,13,14 This issue is especially concerning for critical procedures such as suctioning, where delays or errors can lead to severe outcomes, such as tracheal damage or hemodynamic instability.15 Furthermore, emergency scenarios require healthcare professionals to apply critical thinking and swift interventions—skills that are challenging to develop without adequate training.
Simulation-based training has emerged as an effective strategy to address these gaps, providing a safe and controlled environment to enhance skill development and decision-making.16 High-fidelity manikins (HFMs) replicate realistic patient scenarios, offering structured and standardized learning opportunities for tracheostomy care.17 Physical fidelity in HFMs allows learners to practice procedural tasks such as suctioning, but their inability to simulate patient responses like coughing or emotional interactions limits their realism. Standardized patients are individuals trained to consistently simulate real patient cases for healthcare education, assessment, and research, ensuring a controlled and reproducible learning experience.18 While they can enhance emotional engagement, they lack physical fidelity as they cannot replicate the functional anatomy of a tracheostomy.19–21
Hybrid simulation approaches, which integrate the strengths of HFMs and standardized patients, represent a promising solution. For example, AvTrach® wearable artificial airway simulators (AWAS) enhance standardized patients with functional tracheostomy anatomy, enabling realistic and dynamic training scenarios.22 This approach aligns with conceptual fidelity by presenting realistic clinical cues that enhance decision-making and procedural accuracy. Furthermore, the dynamic feedback provided by AWAS enhances psychological fidelity by fostering learner engagement and immersion. These simulators allow learners to practice hands-on skills while engaging with realistic patient interactions, enhancing clinical competency and self-efficacy.17 Despite these advancements, limited evidence exists on the impact of AWAS on knowledge acquisition, competency, and stress management in high-pressure scenarios like tracheostomy suctioning.
Stress during training is an important consideration, as simulation-based learning can elicit physiological stress responses that rival or exceed those experienced in clinical practice.23 Cortisol levels, a biomarker of physiological stress, provide a useful measure for assessing how individuals cope with high-pressure scenarios.15,24–26 Monitoring cortisol during training offers insights into the interplay between stress and performance, enabling educators to tailor training for optimal outcomes.
This study hypothesizes that training with a wearable artificial airway simulator will lead to superior tracheostomy competency scores compared to HFMs, particularly in clinical settings. It also posits that AWAS training induces higher stress levels during simulation but promotes better stress management in clinical practice, whereas HFM training elicits lower stress in training but higher stress in real-world scenarios. By explicitly considering physical, conceptual, and psychological fidelity, this research aims to provide actionable insights into optimizing tracheostomy care training and enhancing healthcare professionals’ preparedness for complex clinical situations.
The Study
Objective
To compare the effectiveness of a wearable artificial airway simulator on standardized patients (experimental group) versus a high-fidelity manikin (control group) in improving tracheostomy suctioning competency, managing physiological stress (measured through salivary cortisol), and enhancing perceived engagement through dimensions of physical, conceptual, and psychological fidelity among healthcare professionals.
Methods
Design
This study employed a multi-institutional, non-blinded, randomized controlled trial (RCT) design with a 1:1 allocation ratio to compare the effectiveness of two training modalities: an AWAS used on standardized patients (experimental group) and a HFM (control group). The study was conducted between 2017 and 2022 at two completely independent academic tertiary care centers to ensure a diverse and representative sample of clinical environments. The methodology adhered to the Consolidated Standards of Reporting Trials (CONSORT) guidelines.27 to maintain rigor and transparency.
Setting
The study was conducted at two academic tertiary care centers, Johns Hopkins University and the Durham Veterans Affairs Hospital, selected for their diverse clinical environments and advanced simulation facilities. Training sessions were held in simulation laboratories equipped with HFM and AWAS, providing controlled environments for hands-on practice, skill assessment, and group debriefings. Clinical demonstrations were conducted in inpatient units, where participants performed supervised tracheostomy suctioning on real patients, ensuring alignment with routine care schedules and safety protocols.
Ethical Approval
Prior to the initiation of the study, ethical clearance was secured from the Institutional Review Boards (IRBs) at both Johns Hopkins Medicine and the Durham Veterans Affairs. All participants provided informed consent before enrollment, and the study followed ethical principles outlined in the Declaration of Helsinki.
Participants
The study recruited healthcare professionals and students from a variety of disciplines to ensure a comprehensive evaluation of the training modalities. The inclusion criteria were: individuals enrolled in pre-licensure or training programs for nursing, respiratory therapy, physical therapy, and speech-language pathology; and recently graduated healthcare professionals or practicing professionals with an expressed interest or intention to care for patients with a tracheostomy. Participants were categorized as: Novice Professionals, defined as individuals currently in training or with leass than one year of experience in their respective professions. Novices typically had limited clinical exposure and relied primarily on foundational knowledge and structured guidance. Experienced Professionals were defined as those with more than one year of clinical practice, demonstrating proficiency, autonomy, and critical decision-making skills through years of direct patient care and professional development. Healthcare professionals who had performed tracheostomy suctioning on more than three occasions within the preceding 12 months were excluded. This criterion ensured the study focused on participants who would most benefit from the training and minimized the influence of prior advanced experience.
Interventions
This study utilized a structured, multi-session design to evaluate the impact of two training modalities on tracheostomy suctioning competency and physiological stress. Table 1 outlines the timing and sequence of cortisol sample collections across the four sessions, which included recruitment, training, simulation, and clinical demonstrations. Each session incorporated specific activities designed to assess and enhance participants’ skills while monitoring stress responses.
Session 1: Recruitment and Enrollment
Prospective participants expressing interest in the study scheduled individual appointments with the primary investigator or study team at a mutually convenient time and location. During this session, a comprehensive informed consent process was conducted to ensure participants fully understood the study’s purpose, procedures, risks, and benefits. Participants were given ample time to review the consent form and ask questions. If preferred, individuals could take the form home for further consideration and return later to complete the consent process. Once consent was obtained, participants completed a Demographic Questionnaire, which included questions about their professional background and a self-reported comfort level with tracheostomy suctioning on a 0 to 10 scale (0 = no comfort; 10 = complete comfort). This measure provided insight into their baseline confidence in performing the procedure. Following this, salivary cortisol samples (Specimen 1) were collected to serve as an initial reference for physiological stress levels.
Subjective Stress, Salivary Cortisol, and Electrophysiological Responses to Psychological Stress
Experimental Group: AvTrach® Wearable Airway Simulator
The experimental group trained using the AWAS, a device that integrates anatomical realism with interactive feedback. The AWAS features a chest plate secured over a standardized patient, replicating tracheostomy anatomy for tube insertion and suctioning. It includes a reservoir for artificial secretions and a robotic system that detects carina stimulation, providing cues for the standardized patients to respond with coughing and expressions of discomfort. The simulator also emits diverse, remotely controlled breath sounds, allowing participants to practice auscultation and assess the need for suctioning. By combining tactile feedback, auditory cues, and dynamic standardized patient interaction, the AWAS offers an immersive and realistic training experience. AvTrach® is the first and only wearable tracheostomy simulator of its kind, uniquely designed to enhance both procedural and experiential learning in tracheostomy care.22
Control Group: Laerdal High Fidelity Manikin
The control group trained with the Laerdal HFM, which replicates an anatomically accurate tracheostomy site for practicing suctioning, airway maintenance, and secretion clearance. Programmable breathing patterns simulated various respiratory conditions, allowing participants to respond to clinical scenarios like airway obstruction. While the HFM provided a standardized environment for technical skill development, the device used for the study lacked interactive feedback, such as patient responses to discomfort, focusing primarily on procedural training.
Participants in both groups observed a standardized demonstration of tracheostomy suctioning by an instructor, following the competency checklist. They then practiced on their assigned training modality, HFM or AWAS, with instructors available for guidance and feedback. Salivary cortisol samples were collected immediately after training (Specimen 3) and 15 minutes later (Specimen 4) to assess physiological stress. This session combined theoretical instruction, hands-on practice, and stress monitoring to evaluate training effectiveness comprehensively.
Session 3: Simulation Competency and Stress Levels
Fifteen minutes before the scheduled simulation demonstration, participants provided a pre-demonstration salivary cortisol sample (Specimen 5). Each participant then demonstrated tracheostomy suctioning on their assigned modality, HFM or AWAS, while an instructor assessed their performance using a standardized competency checklist. After the demonstration, participants provided a salivary sample (Specimen 6) to measure stress response and received formative feedback. Another cortisol sample (Specimen 7) was collected 15 minutes later to assess stress recovery. This session combined skill application with stress evaluation, highlighting the training interventions’ impact on performance and stress dynamics.
Session 4: Clinical Competency and Stress Levels
Within two weeks of the second session, participants reconvened at predetermined clinical settings depending on patient availability to perform tracheostomy suctioning on patients, aligning with routine care schedules to ensure standard care was maintained. To ensure consistency, sessions were scheduled at the same time of day as earlier sessions. Participants provided a pre-demonstration salivary cortisol sample (Specimen 8), performed suctioning under observation using a competency checklist, and provided immediate post-demonstration (Specimen 9) and recovery (Specimen 10) cortisol samples. This session simulated real-world clinical conditions, evaluating participants’ skills and stress responses in a healthcare setting.
Outcomes
Comfort level: Comfort level was assessed using a single-item self-reported measure that asked participants to rate their confidence in performing tracheostomy suctioning on a non-ventilated patient. Participants rated their comfort on a 0 to 10 Likert scale, where 0 indicated no comfort, and 10 indicated complete confidence. This measure provided a baseline and post-training indicator of participants’ self-perceived readiness and confidence.
Tracheostomy competency scores: Competency in tracheostomy suctioning was evaluated using an objective structured clinical evaluation (OSCE) tool, which was developed and validated through the Delphi technique to ensure consensus among experts in clinical care and simulation.28 This assessment captured key elements of physical, conceptual, and psychological fidelity:
-
Physical Fidelity: The OSCE tool measured participants’ interaction with the physical components of the simulation, including accurate suctioning techniques and proper handling of equipment.
-
Conceptual Fidelity: The tool evaluated whether participants effectively responded to the clinical cues provided by the simulation, including decision-making and procedural accuracy.
-
Psychological Fidelity: The evaluation captured participants’ ability to remain engaged and emotionally invested in the scenario, simulating the mental and emotional demands of real patient care.
Standardized video scenarios were used to train evaluators, with four sessions conducted at Johns Hopkins University and two at Durham Veterans Affairs. Inter-rater reliability demonstrated moderate to substantial agreement, with Cohen’s Kappa coefficients of 0.49, 0.59, and 0.78 across three testing videos, confirming the tool’s consistency and validity for competency evaluation.
Cortisol levels: Salivary cortisol, a validated biomarker for physiological stress, was used to measure participants’ stress responses throughout the study.24,26 To account for the delayed peak of cortisol secretion following stress activation, salivary cortisol was collected immediately after training and demonstrations, as well as 15 minutes post-event. While immediate samples provide insight into acute physiological changes, 15-minute post-event measurements are likely to reflect peak cortisol levels based on established findings that cortisol peaks 10–30 minutes after stress cessation.29 Sampling was standardized to control for circadian variations, as cortisol levels fluctuate naturally throughout the day.25 Ten samples were collected using Salivette collection devices at predefined intervals (Table 1). Participants followed a strict protocol: tilting the test tube to release the swab, rolling it in their mouth for two minutes without chewing or touching it with their fingers, and returning it to the tube. Samples were immediately sealed, labeled, and stored at -40°C before laboratory analysis, ensuring sample integrity. Laboratory analysis utilized a high-sensitivity enzyme immunoassay (Cat. No. 1-3002), with a detection sensitivity of 0.007 μg/dL and a standard curve range of 0.012–3.0 μg/dL.30 Quality control demonstrated high accuracy, with intra-assay and inter-assay coefficients of variation at 4.60% and 6.00%, respectively.23,31
Dimensions of Fidelity
The outcomes of the study were framed within the dimensions of fidelity (physical, conceptual, and psychological).32
-
Physical Fidelity: Both the AWAS and the HFM provided anatomically accurate representations of tracheostomy procedures.33 However, the AWAS enhanced tactile feedback and added dynamic responses, such as coughing and discomfort, offering greater physical engagement.
-
Conceptual Fidelity: The AWAS provided clinical cues, such as auscultation findings and secretion levels, that closely aligned with real-life scenarios, supporting procedural accuracy and decision-making.33
-
Psychological Fidelity: Participants using the AWAS reported higher engagement and emotional investment, reflecting enhanced immersion in the training environment. These factors likely contributed to their improved stress management and skill retention, as observed in the study’s measured outcomes.33
Changes to Outcomes
During the trial, research assistants noted participants’ anecdotal feedback describing the AWAS as providing an authentic and engaging experience. This observation aligns with the INACSL Standards’ emphasis on psychological fidelity, which prioritizes immersion and emotional engagement as critical factors in simulation-based education.34 However, qualitative data supporting this claim were not systematically collected, and future studies should incorporate such methods to strengthen findings related to participant experience.
Sample Size Calculation
The sample size was calculated based on salivary cortisol levels, requiring 60 participants (30 per group) to achieve 80% power, assuming a moderate effect size of 0.41, a significance level of 0.05, and a 0.5 correlation among repeated measures. To account for a 10% attrition rate, the enrollment target was increased to 70 participants, ensuring sufficient power and resilience against potential dropouts.
Randomization
Simple randomization was performed using the RAND function in Microsoft Excel to ensure unbiased allocation of participants to either the intervention or control group. The randomization procedure was overseen by the principal investigator, who maintained the allocation sequence in a password-protected computer folder to safeguard its integrity. To prevent potential bias, the group assignments were concealed from the study team until participants had provided informed consent and their initial salivary cortisol sample. The study coordinator managed participant enrollment, retrieving allocation information from the principal investigator only after eligibility was confirmed and the baseline data collection was complete. This sequential process ensured that randomization was both secure and transparent, minimizing the risk of allocation bias and maintaining rigor throughout the study.
Blinding
Blinding of participants was not feasible due to the distinct nature of the training modalities and the visible differences between the devices used for evaluation (HFM versus AWAS). To address this limitation, randomization process was conducted securely and independently, and the study team adhered to standardized protocols for training, evaluation, and feedback to maintain consistency across groups. The lack of participant blinding was explicitly acknowledged in the study design, with a focus on mitigating its potential impact through objective assessment tools and controlled evaluation conditions.
Statistical Methods
Descriptive statistics were used to summarize demographic data, with medians and interquartile ranges reported for continuous variables and frequencies and percentages for categorical variables. Baseline comfort levels were analyzed using means and standard deviations. Group comparisons were performed using the Wilcoxon rank-sum test for non-parametric variables and tracheostomy competency scores, chi-square tests for categorical variables, and two-sample t-tests with equal variances for baseline comfort levels. To evaluate cortisol level differences between groups while controlling for baseline comfort, a mixed-effects regression model was applied, accounting for repeated measures.
Results
Participant Recruitment and Retention
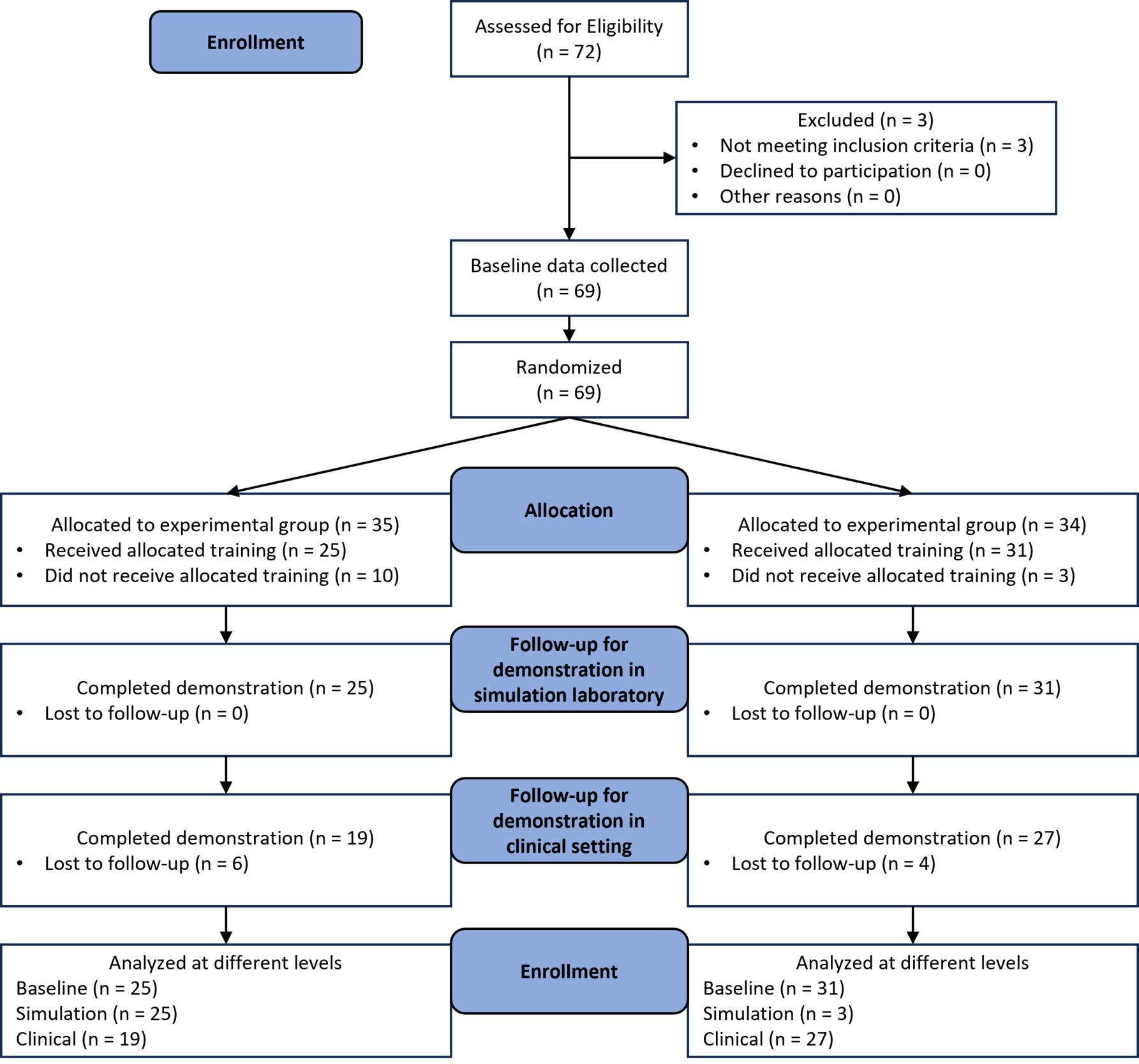
The study began in July 2017, assessing 72 participants for eligibility and excluding 3 who did not meet the criteria because they had more experience (Figure 1).Baseline data were collected from 69 participants, randomized into the control group (n = 35) or experimental group (n = 34). Of these, 25 control group participants and 31 experimental group participants completed the allocated training, with 10 and 3 participants, respectively, withdrawing before training. In follow-up assessments, 25 control group participants completed the simulation laboratory demonstration, and 19 completed the clinical demonstration, with 6 lost to follow-up. In the experimental group, 31 participants completed the simulation demonstration, and 27 completed the clinical demonstration, with 4 lost to follow-up. Attrition was due to scheduling conflicts, lack of interest, clinical commitments, and COVID-19-related disruptions. Final follow-up attempts concluded in June 2022, highlighting challenges in maintaining engagement over the study’s duration.
Participants characteristics
The study enrolled 69 participants, representing a diverse cohort with a median age of 28 years (IQR: 25–39) and an age range spanning 22 to 63 years. Gender distribution included 13 men (18.8%), 55 women (79.7%), and 1 participant identifying as transgender (1.5%). Regarding ethnicity, 5 participants (7.3%) identified as Hispanic or Latino, while 64 participants (92.7%) identified as non-Hispanic or non-Latino. The racial composition included 46 Caucasians (66.7%), 12 African Americans (17.4%), and 11 Asians (15.9%). Participants’ professional backgrounds varied, with 45 (65.2%) being student nurses, 12 (17.4%) experienced nurses, 9 (13.0%) novice nurses, 2 (2.9%) physical therapists, and 1 (1.5%) speech-language pathologist. There were no statistically significant differences in demographic or professional characteristics between the control group (n = 35) and the intervention group (n = 34), ensuring baseline comparability (Table 2).
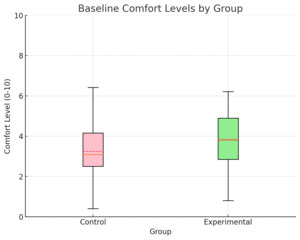
Baseline comfort levels
Participants reported an overall mean comfort level of 3.7 ± 1.6 on a 0–10 scale, where 0 indicated no comfort and 10 indicated complete comfort with tracheostomy suctioning (Figure 2). A two-sample t-test comparing baseline comfort levels between the control group (n = 35) and the experimental group (n = 34) revealed no statistically significant difference. The mean comfort score in the control group was 3.46 (SD = 1.60), while the intervention group reported a slightly higher mean score of 4.00 (SD = 1.63); p = 0.17. These findings indicate comparable baseline comfort levels between the two groups, ensuring that any observed differences in outcomes are unlikely to be attributable to initial comfort disparities.
Comparison of Tracheostomy Competency
Baseline competency scores were similar between the control group (median = 21, IQR: 15–23) and the experimental group (median = 20, IQR: 18–22; p = 0.60) (Figure 3; Supplemental Tables 1–3). Following training, both groups showed significant improvements in competency during post-training demonstrations. In the simulation laboratory, the control group, trained with a HFM, achieved a median score of 31 (IQR: 28–31), while the experimental group, trained with the AWAS on standardized patients, achieved a slightly higher median score of 32 (IQR: 31–32; p = 0.01). In the clinical setting, the control group scored 30 (IQR: 27–31), whereas the experimental group significantly outperformed with a median score of 34 (IQR: 33–35; p < 0.001).
Both groups showed improvement from pre-training to post-training assessments (p < 0.001). However, the transition from post-training to clinical demonstrations revealed a stark contrast. The control group exhibited no significant improvement (p = 0.99), while the experimental group demonstrated a significant increase in competency (p < 0.001). The change in competency scores from pre-training to post-training was not significantly different between the groups (p = 0.10), controlling for comfort levels. However, a significant difference was observed when comparing the change in scores from post-training simulation to clinical demonstrations, favoring the experimental group (p = 0.007).
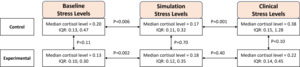
Comparison of cortisol levels
Post-training cortisol levels were comparable between the control group (median = 0.20, IQR: 0.13–0.47) and the experimental group (median = 0.13, IQR: 0.10–0.30; p = 0.11) (Figure 4). In the simulation laboratory, cortisol levels remained similar: 0.17 (IQR: 0.11–0.32) for the control group and 0.18 (IQR: 0.12–0.35) for the experimental group (p = 0.70). In the clinical setting, the control group had higher cortisol levels (median = 0.38, IQR: 0.15–1.28) compared to the experimental group (median = 0.22, IQR: 0.14–0.45; p = 0.10).
Within-group analyses showed significant increases in cortisol levels from post-training to simulation demonstrations in both groups: control (p = 0.006) and experimental (p = 0.002). Cortisol levels further increased from simulation to clinical demonstrations in the control group (p = 0.001) but remained stable in the experimental group (p = 0.40), indicating better stress adaptation. Between-group comparisons revealed significant differences in cortisol changes. The control group experienced larger increases in cortisol levels from post-training to simulation demonstrations (p < 0.001) and from simulation to clinical demonstrations (p = 0.006).
Engagement and Feedback
Although the study did not directly measure psychological fidelity, participants in the AWAS group anecdotally described their training as more interactive and engaging. Observations from research assistants also highlighted the enhanced immersion and emotional investment of participants in the experimental group.
Discussion
This randomized controlled trial provides important insights into the effectiveness of two simulation-based training modalities—a HFM and an AWAS used on standardized patients—for enhancing tracheostomy suctioning competency and managing physiological stress among healthcare professionals. Both training modalities demonstrated significant improvements in competency scores post-training. However, the experimental group trained with the AWAS exhibited superior outcomes in clinical settings and demonstrated better stress adaptation compared to the control group trained with the HFM. These results highlight the critical role of fidelity in simulation-based training, particularly for complex and high-stakes procedures like tracheostomy suctioning. The findings highlight how the AWAS, through its innovative design, enhances physical, conceptual, and psychological fidelity, enabling learners to develop the skills and confidence needed to perform tracheostomy suctioning accurately and effectively in real-world clinical scenarios.
Physical Fidelity in Tracheostomy Suctioning
Physical fidelity encompasses the anatomical and procedural realism provided by simulation tools. The HFM used in the study offered a static yet precise representation of the tracheostomy site, enabling learners to practice technical skills like suctioning and secretion clearance. However, the AWAS provided an enhanced physical fidelity experience by incorporating tactile feedback, dynamic responses such as coughing, and auditory cues like breath sounds. These features replicated patient anatomy and physiology more effectively, bridging the gap between simulated and real-world conditions. Findings from a systematic review of 14 randomized and 5 case controlled studies support the assertion that high physical fidelity improves confidence and technical skills, particularly for procedures requiring intricate manual dexterity.35 Similarly, participants in the AWAS group of this study demonstrated superior clinical competency scores compared to the HFM group, suggesting that enhanced physical fidelity not only improves skill acquisition but also translates into better real-world performance. Despite these benefits, studies highlight that the costs and logistical complexities of high-fidelity tools remain significant barriers to widespread implementation.35,36
Conceptual Fidelity in Tracheostomy Suctioning
Conceptual fidelity ensures that all elements of a simulation scenario—such as clinical cues, patient symptoms, and procedural outcomes—are logically aligned, enabling learners to integrate theoretical knowledge into practice. Both the HFM and AWAS modalities adhered to this principle by presenting clinically relevant scenarios, including airway obstruction and secretion management. A qualitative study of participants from the Interprofessional Simulations of Patient Experiences Across the Care Continuum-Child and Youth course emphasized that high conceptual fidelity supports effective clinical learning by aligning the training environment with professional roles and decision-making processes.12 In our study, the AWAS group’s significant improvement in competency scores during clinical demonstrations supports this finding, as participants could better apply learned skills to dynamic patient interactions. Focus group study of 27 medical and 18 nursing students in Newcastle and Oxford, UK revealed that conceptual fidelity enhances understanding of complex clinical situations, making learners more adept at addressing unexpected challenges—a benefit mirrored in the AWAS group’s stress management and performance outcomes.36
Psychological Fidelity in Tracheostomy Suctioning
Psychological fidelity, which involves creating a realistic and emotionally engaging training environment, was a defining strength of the AWAS modality. By integrating standardized patients capable of responding dynamically to suctioning actions (e.g., coughing and expressing discomfort), the AWAS fostered greater emotional investment and professional role adoption. Participants reported feeling more immersed and prepared for real-world challenges, which was reflected in their superior stress regulation during clinical demonstrations. The heightened psychological fidelity of the AWAS group demonstrated that emotionally engaging scenarios promote better decision-making and task management under pressure.37 Similarly, another study reported that interprofessional simulations enhance psychological fidelity by replicating team dynamics and fostering authentic professional interactions.36 Our study’s cortisol analyses provide quantitative evidence of this effect: while both groups experienced stress increases during simulation, the AWAS group demonstrated better stress adaptation during clinical demonstrations. High psychological fidelity elicits stronger emotional and cognitive engagement, which, although initially stressful, ultimately enhances skill retention and preparedness for high-stakes scenarios.35
Integration of Fidelity Dimensions
This study highlights the importance of integrating physical, conceptual, and psychological fidelity to optimize simulation-based training. The AWAS modality effectively combined all three dimensions, providing participants with a comprehensive learning experience. Participants not only demonstrated improved technical and decision-making skills but also exhibited enhanced stress resilience, a critical competency for managing emergencies like tracheostomy tube dislodgement or airway obstruction. The integration of these fidelity dimensions is essential for designing impactful simulations that align with institutional goals and learner needs.34 By contrast, the HFM modality, while effective in improving technical skills, lacked the dynamic feedback and emotional engagement necessary to replicate real-world complexities fully. This aligns with findings from interviews of 10 participants from the Interprofessional Simulations of Patient Experiences Across the Care Continuum - Child and Youth course that physical fidelity alone is insufficient to achieve optimal learning outcomes without the support of psychological and conceptual elements.12
Optimizing Stress Resilience and Clinical Performance
Stress management is essential in simulation-based training (SBT) for high-stakes procedures like tracheostomy care. This study demonstrated that participants trained with the AWAS exhibited better stress resilience, as shown by stable cortisol levels during clinical demonstrations, compared to those trained with HFMs. Elevated cortisol levels during AWAS training mirrored real-world stress responses, helping participants acclimate to clinical pressures. Martínez-Pascual and team similarly observed anticipatory stress responses during OSCEs, emphasizing the role of controlled stress exposure in building resilience.38
While both groups experienced stress increases post-training, the HFM group showed significantly elevated cortisol levels during clinical scenarios, suggesting incomplete stress adaptation. In contrast, the AWAS group’s stable cortisol levels indicate its effectiveness in replicating procedural and emotional challenges. These findings align with Lin et al. (2022), who noted the impact of stress exposure on cortisol dynamics, and Mendes et al. (2022), who linked academic stress to elevated cortisol.39,40 Anton et al. (2021) found that physiological stress markers negatively correlate with simulation performance, while Sigwalt et al. (2020) demonstrated that stress management training enhances readiness for clinical challenges.41,42 AWAS’s integration of physical, conceptual, and psychological fidelity further supports skill acquisition and emotional resilience. Wong et al. (2023) and Ferreira et al. (2020) similarly highlighted the benefits of stress reduction and confidence-building in improving performance.43,44 This study emphasizes the value of dynamic, immersive training like AWAS, which balances stress levels to foster stress resilience and clinical competency. By supporting gradual acclimatization through realistic scenarios, AWAS facilitates smoother transitions to practice. These findings align with Cavaleri et al. (2023) and Martínez-Pascual et al. (2022), who advocate for structured, tailored stress exposure to optimize learning outcomes and preparedness for real-world challenges.38,45
Implications for Tracheostomy Care Practice, Research, and Policy
The integration of AWAS into interprofessional education has transformative implications for tracheostomy care. This study demonstrated that AWAS-based training enhances not only technical skills but also emotional preparedness, addressing critical dimensions of physical, conceptual, and psychological fidelity. By providing dynamic feedback, such as tactile cues and patient-like responses, AWAS equips nurses, respiratory therapists, and other healthcare professionals with the ability to perform tracheostomy suctioning while managing the emotional complexities of patient care. This holistic approach helps learners practice not only procedural techniques but also empathetic communication and reassurance, crucial for alleviating the anxiety experienced by patients and their families during tracheostomy care.46–48 The interprofessional application of AWAS fosters collaboration, enabling teams to refine their responses to the multifaceted needs of patients in high-stakes situations.49,50
In research, this study highlights the need to explore the long-term retention of tracheostomy care skills acquired through AWAS. Future studies should examine how these training benefits persist over time and across diverse healthcare settings.51,52 Additionally, the AWAS model offers potential for broader applications, such as managing tracheostomy-related emergencies, including tube dislodgement, false tracts, and airway obstructions.3,4,53 Investigating these scenarios could deepen healthcare professionals’ understanding of emergency management and critical care, with implications for allied health disciplines. Further research is also needed to evaluate the scalability of AWAS in resource-limited environments and its cost-effectiveness compared to traditional training modalities. Expanding its use to address infection control challenges in aerosol-generating procedures would also enhance its relevance in contemporary practice.54,55
From a policy perspective, implementing AWAS in training programs for interprofessional teams can set a new standard for tracheostomy education. Policymakers should prioritize funding for technologies that integrate physical, conceptual, and psychological fidelity to improve safety and efficacy in tracheostomy care.12,35,49,50 Scaling these programs across varied healthcare settings will require investments in simulation infrastructure and support for faculty training. Additionally, incorporating AWAS into interprofessional education initiatives can strengthen team-based care, enhancing collaboration between nurses, respiratory therapists, speech-language pathologists, and physicians.5 By equipping healthcare teams with comprehensive training tools, AWAS has the potential to improve patient safety, clinical outcomes, and overall satisfaction in tracheostomy management.
Limitations
This study has several limitations. First, the non-blinded design may have introduced bias, as participants and researchers were aware of group assignments. Second, the relatively small sample size may limit the generalizability of the findings. Third, the study focused on short-term competency and stress levels, without assessing long-term retention of skills or stress resilience. Fourth, while salivary cortisol was used as a primary measure of stress, it may not fully capture the complexity of physiological and emotional stress responses. Other factors, such as sleep quality, medication use, diet, and physical activity, can influence salivary cortisol levels and were not systematically controlled for. Furthermore, the study period overlapped with the COVID-19 pandemic, which may have influenced participant stress levels. While baseline cortisol levels were measured, the potential impact of the pandemic on participants’ overall stress and well-being was not specifically assessed. Finally, the study did not account for potential practice effects. Participants may have had opportunities to perform tracheostomy suctioning outside of the study protocol during the two-week intervals between sessions. Such additional practice could have influenced their competency and stress levels, potentially confounding the results. Additionally, while baseline comfort levels were assessed, they were not re-evaluated at subsequent time points. This limits the ability to demonstrate changes in comfort over time and assess the differential impact of the interventions on participant confidence.
Conclusion
This study demonstrates the effectiveness of AvTrach® wearable artificial airway simulators (AWAS) in enhancing tracheostomy suctioning competency and stress management compared to high-fidelity manikins (HFM). By integrating physical, conceptual, and psychological fidelity, AWAS provides an immersive training experience that prepares healthcare professionals for the technical and emotional challenges of tracheostomy care. The findings emphasize AWAS’s potential in interprofessional education, fostering collaboration among nurses, respiratory therapists, and speech-language pathologists to improve patient outcomes. Future research should evaluate long-term skill retention, scalability, and applications in tracheostomy emergencies and other critical care scenarios. By integrating AWAS into training programs, educators and policymakers can set a new standard for comprehensive, team-based tracheostomy care.
Conflicts of interest
The authors declare no conflicts of interest.
Funding
-
Quod Erat Demonstrandum (QED) Innovation Subaward via the University of Delaware
-
Agency for Healthcare Research and Quality (5R18HS029124) for Center for Immersive Learning and Digital Innovation: A Patient Safety Learning Lab advancing patient safety through design, systems engineering, and health services research
Corresponding Author
Vinciya Pandian, PhD, MBA, MSN, ACNP-BC, FCCM, FAANP, FAAN, FFNMRCSI
Associate Dean of Graduate Education and Professor of Nursing and Joint Faculty of Department of Otolaryngology-Head and Neck Surgery, College of Medicine
Executive Director, Center for Immersive Learning and Digital Innovation
Ross and Carol Nese College of Nursing, The Pennsylvania State University, University Park, PA, United States
President, Global Tracheostomy Collaborative, Chicago, IL, United States
Email: vpandian@psu.edu
Phone: 443065503482
Acknowledgement
The authors would like to acknowledge Mary Holtschneider, Kelly Cunningham, and Abbie Homan for their assistance with data collection, and Dr. Nancy Perrin for guidance with statistical analysis.
Statistical Responsibility Statement
The author(s) affirm that the methods used in the data analyses are suitably applied to their data within their study design and context, and the statistical findings have been implemented and interpreted correctly.