INTRODUCTION
The increasing complexity of patient conditions and the healthcare system has led to a wider range of indications for tracheostomy. These include prolonged mechanical ventilation, upper airway obstruction, airway protection, and the need for pulmonary hygiene. Over 20 million adults globally require intensive respiratory support annually,1 with approximately 250,000 individuals undergoing tracheostomy primarily after invasive ventilation for critical illness.2,3 Although tracheostomies are generally beneficial in reducing sedation and enhancing patient comfort and autonomy, they also carry significant risks including procedure-related adverse events and post-tracheostomy care complications.4–6 Adverse events such as dislodgement, occlusion, or bleeding account for a substantial proportion of airway-related deaths and hypoxic brain injuries in healthcare settings and the community, yet much of this harm is preventable.7–9 These observations highlight the need for a deeper understanding of gaps in tracheostomy care and effective prevention strategies.
Historically, emphasis has been placed on the timing, technique, and indication of tracheostomies.10–15 Despite increasing awareness of these practices, critical gaps persist in key areas such as workforce training, care partner (families and caregivers) support, and equitable access to care. Most tracheostomy-related adverse events stem from gaps in managing tracheostomy care rather than from the procedure itself.7,16 Understanding these issues with tracheostomy care requires a broad stakeholder engagement—a perspective that has been largely overlooked in previous studies.17 This gap contributes to the lack of targeted strategies and resources available to improve the safety and quality of life for tracheostomy patients.
Furthermore, tracheostomy care spans several disciplines, necessitating collaboration among physicians, nurses, respiratory therapists, physiotherapists, speech-language therapists, dieticians, and psychologists.18,19 Multi-institutional studies have demonstrated the benefits of an integrated approach to care, including reductions in mortality, adverse events, and costs, as well as quicker transitions to eating and speaking for patients, along with improved mental health outcomes.20,21 Further integration with care partners can help reduce gaps in airway management and tracheostomy complications, ultimately improving safety and quality of care.22,23
The purpose of this study was to identify critical gaps in tracheostomy care, focusing on education, workforce competency, access, affordability, and caregiver empowerment, through a multi-stakeholder global survey. By exploring the perspectives of healthcare professionals, patients, and caregivers, the study aimed to provide actionable insights for implementing standardized training, enhancing care coordination, and improving equitable access to tracheostomy care globally.
MATERIALS AND METHODS
Study design
A cross-sectional, descriptive study was conducted using an anonymous online survey. This survey explored challenges in tracheostomy care, barriers to training and retaining adequate numbers of healthcare professionals (HCP) with expertise in tracheostomy care, and problems with access to and affordability related to tracheostomy care. The Checklist for Reporting Results of Internet E-Surveys (CHERRIES) was used to report findings.24,25
Ethical review
The protocol was reviewed and approved by the Johns Hopkins Medicine Institutional Review Board (IRB00354548), ensuring alignment with ethical standards and institutional policies.
Survey development
A 19-item survey (Supplemental Figure 1) was developed by an interprofessional team of HCP, patients, and family members, reflecting a participatory approach. Each survey item was carefully designed to align with the study’s objectives of identifying gaps in education, workforce competency, caregiver support, access, and affordability in tracheostomy care. Items were mapped to key domains identified in prior research and practice guidelines, such as the Global Tracheostomy Collaborative’s (GTC) quality improvement framework and other validated needs-assessment tools.7,26
To ensure the rigor and reliability of the survey, the survey underwent iterative cycles of review with feedback from the larger GTC community, ensuring broad input and relevance.26–28 The survey instrument was built using Qualtrics software, version 2020 (Qualtrics, Provo, UT).29 To mitigate the risk of bias and ambiguity, a quality checklist was employed to vet the survey questions, identifying, and eliminating potential design flaws such as leading questions, double-barrel questions, and inadequate response options. This vetting process ensured that the survey questions were clear, unbiased, and capable of eliciting accurate and meaningful responses. The survey’s pre-testing and piloting stages involved evaluating questions for clarity and relevance.
Participant sample
Participants from the GTC Learning Community were invited to take part in the survey through email outreach.30 The GTC has maintained a secure registry of patients, families, and HCP involved in its educational and quality improvement initiatives since its establishment in 2012.7 Membership in this learning community is cultivated through interest group forums, global webinars, international tracheostomy symposia, or referrals from patient-focused networks. Individuals who register have the option to receive newsletters, updates, and survey invitations. Survey respondents were queried about their primary identification among the listed stakeholders within the learning community, which encompassed patients, families, caregivers, social workers, hospital administrators, and a wide range of HCP.
Survey administration
The survey was distributed electronically to members of the GTC Learning Community through a listserv. Two follow-up invitations were sent over two-week intervals, with the survey closing after four weeks. Participation was voluntary. The survey was administered online using the Qualtrics online survey platform.29 Participants accessed the survey through a unique link provided in the study recruitment materials. To prevent multiple responses from the same individual, internet protocol limits were implemented.
Survey questionnaire and outcome measures
The survey included six structured demographic questions followed by six questions evaluating tracheostomy care challenges, availability of HCP with expertise in tracheostomy, access to care, and affordability concerns. Participants rated the severity of issues on a sliding scale ranging from 0 to 10 (0=not a problem and 10=severe problem). The remaining seven multiple-choice questions captured qualitative insights regarding the issues the respondents rated on the sliding scale, with an option of “other” with free-text option.
Data collection
Data were collected and stored with the Qualtrics online survey platform.31 Aggregate, de-identified survey responses were stored on a secure, password-protected server with two-factor authentication behind the institutional firewall. Only de-identified data were downloaded into an Excel spreadsheet for data cleaning and analysis, with data quality checks to ensure completeness.
Statistical analysis and qualitative synthesis
We analyzed quantitative data descriptively, presenting median and interquartile ranges (IQR) for ordinal variables and counts and percentages for categorical data. While information for each HCP role and caregiver group was reported, we did not conduct statistical comparisons between these groups due to the imbalanced sample sizes. This approach was taken to ensure transparency and avoid overinterpretation of data from underrepresented groups, such as caregivers. Qualitative responses were analyzed for recurring themes, capturing insights on specific tracheostomy care challenges. Missing data were handled by excluding incomplete responses from the analysis. Statistical analysis was conducted using Stata SE 16.0.32
RESULTS
Participant characteristics
The study included 170 participants from diverse professional roles, demographics, and global locations, reflecting the multidisciplinary nature of tracheostomy care (Table 1). The largest professional groups were speech-language pathologists (30%), nurses (24%), respiratory care practitioners (24%), and physicians/surgeons (13%). Other roles included patients (4%), family members/caregivers (4%), and hospital administrators/social workers (1%). Among physicians/surgeons, specialties were anesthesiologists/intensivists (52%), otolaryngologists (26%), interventional pulmonologists (13%), and general practitioners (9%). Most participants were aged 41–65 years (60%), followed by 21–40 years (31%) and over 65 years (9%). Gender distribution showed 82% female, 16% male, and 2% non-binary respondents. Geographically, participants represented 14 countries across six continents, with the majority from the United States (46%), the United Kingdom (22%), Australia (12%), Canada (8%), and India (5%). The remaining 7% were from Israel, New Zealand, Brazil, Germany, Indonesia, Italy, Puerto Rico, South Africa, and Spain. All survey responses were complete, with no exclusions for missing data.
Challenges with tracheostomy care based on severity scores
Respondents rated the importance of various aspects of tracheostomy care on a scale from 0 (“not a problem at all”) to 10 (“severe problem”). The most pressing concern identified was the limited availability of HCP with specialized tracheostomy expertise, which received a median rating of 8 (IQR: 6, 10) (Table 2). This concern was closely followed by access issues for patients in remote areas, with a median score of 7 (IQR: 4, 9). Affordability also emerged as a significant concern, with a median score of 6 (IQR: 4, 8), specifically highlighting costs associated with extended hospital stays and ventilator-associated pneumonia (VAP).
Participants also expressed concerns about challenges related to adverse events and the lack of patient-centered care, particularly in suctioning and stoma maintenance. Suctioning issues, such as discomfort, aspiration, bleeding, and VAP risk, were the highest rated concerns, with a median severity level of 6 (IQR: 3, 7). Stoma care and tracheostomy tube changes were identified as moderately severe challenges, each with median scores of 5 (stoma care: IQR: 4, 7; tube changes: IQR: 3, 7). These challenges included concerns about tube dislodgement, occlusion, false tract formation, trauma, and bleeding.
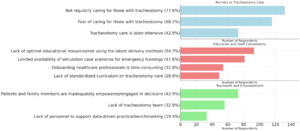
Challenges specific tracheostomy suctioning, tube changes, stoma care, and devices
The issues related to suctioning, tube changes, and stoma care were categorized across professional roles and stakeholders involved in tracheostomy care (Figure 1, Supplemental Table 1).
Suctioning
The most frequently reported concerns were variation in technique (102, 60%) and discomfort (99, 58%), followed by excessive secretions (76, 45%) and inconsistent suctioning schedules (63, 37%). Speech-language pathologists were the primary group reporting concerns about variation in technique (33, 32%) and discomfort (35, 35%), while respiratory therapists (25, 33%) and nurses (23, 30%) expressed notable concerns about excessive secretions. Ventilator-associated pneumonia (39, 23%) and aspiration (29, 17%) were predominantly highlighted by speech-language pathologists (20, 51% and 14, 48%, respectively). Suctioning skills deficits were least reported (9, 5%), primarily by nurses (5, 56%). Free-text comments from 20 respondents (12%) further highlighted issues such as excessive suction pressure and depth, overly frequent suctioning, challenges with secretion management linked to underlying conditions, competency issues, availability of home suctioning devices, inadequate training for nurses, lack of standardized training and competency checks, and limited family education on correct suctioning techniques.
Tube Changes
The most significant concern was a lack of experience or competency (112, 66%), with speech-language pathologists (33, 30%) and respiratory therapists (30, 27%) being the most affected groups. Fear of performing tube changes (77, 45%) was similarly distributed across speech-language pathologists (22, 29%) and nurses (23, 30%). Dislodgement (51, 30%) and occlusion (41, 24%) were reported across various roles, with speech-language pathologists (15, 29% and 16, 39%, respectively) highlighting these issues most frequently. Trauma (35, 21%) and bleeding (29, 17%) were primarily reported by speech-language pathologists (15, 43%) and respiratory therapists (10, 35%). Free-text comments from 23 respondents (14%) cited issues with procedural technique, limited staff availability, coordination of care, and gaps in HCP knowledge.
Stoma Care
Concerns about stoma pressure injury (84, 49%) and stoma infection (80, 47%) were common, particularly among speech-language pathologists (23, 27% and 28, 35%) and respiratory therapists (21, 25% and 20, 25%). Stoma care knowledge deficits (8, 5%) were identified primarily by nurses (5, 66%). These included stoma blockage, inconsistent or inadequate cleaning practices, challenges with moisture management, and variability in stoma care standards. Respondents also emphasized concerns about granulation tissue formation, limited access to essential supplies, and difficulties in obtaining emergency replacement tube sizing. Other concerns involved post-decannulation management, and educational gaps for both patients and HCP. Furthermore, respondents identified systemic challenges, such as lack of community-based support following hospital discharge, healthcare disparities in rural settings, and inadequate availability of pediatric-specific tracheostomy supplies.
Device-Related Concerns
Free-text responses also highlighted device-related concerns, which encompassed a broad range of issues, from placement techniques to perioperative care, and decannulation processes. Respondents highlighted varying approaches to surgical stoma creation, granulation tissue formation, and difficulties in accessing appropriate tracheostomy tubes. Challenges with tube re-insertion were frequently reported, compounded by limited knowledge of tube options among HCP, and inadequate availability of skilled personnel to perform tube changes safely and effectively. Additional concerns included uncertainty around the timing for downsizing or capping tracheostomy tubes, as well as inadequate coordination of decannulation care. The perceived inefficacy of finger occlusion compared to one-way speaking valves was noted as a limitation in current practice. Respondents also identified inconsistencies in decision-making processes among care teams, a lack of contingency planning for unexpected difficulties, and delays in performing both routine and urgent tube changes.
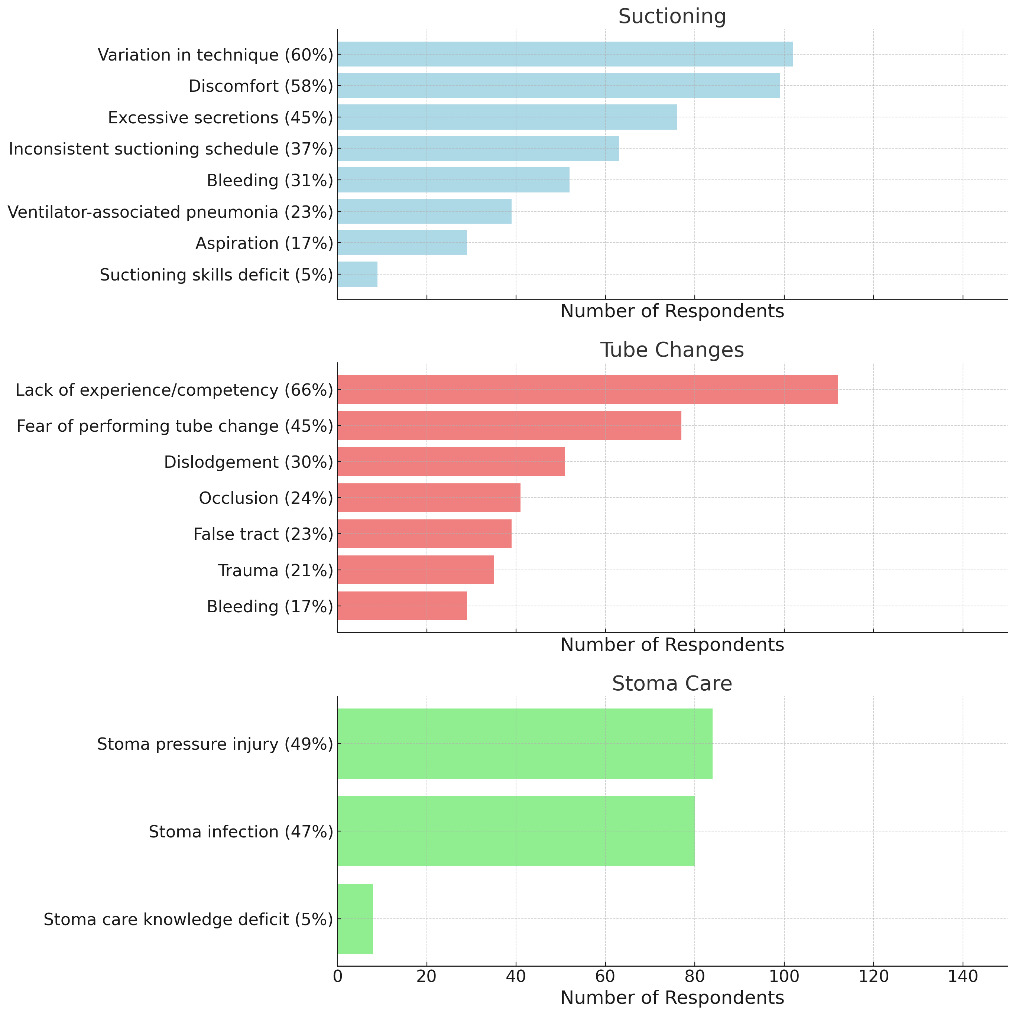
Barriers to Tracheostomy Care: Insights into Education, Competency, Teamwork, and Patient Empowerment
The barriers to tracheostomy care, education, staff competency, teamwork, and patient empowerment were categorized by professional roles and stakeholders, highlighting diverse perspectives and challenges (Figure 2; Supplemental Table 2).
Barriers to Tracheostomy Care
The most frequently reported barrier was not regularly caring for those with tracheostomy (132, 77.6%), with speech-language pathologists (42, 31.8%) and nurses (32, 24.2%) reporting the largest proportions. Other significant barriers included fear of caring for those with tracheostomy (116, 68.2%), with respiratory therapists (33, 28.5%) and speech-language pathologists (34, 29.3%) reporting the highest percentages, and tracheostomy care being labor-intensive (73, 42.9%), predominantly noted by speech-language pathologists (26, 35.6%).
Education and Staff Competency
A lack of optimal educational resources or not using the latest delivery methods (93, 54.7%) was a key challenge, reported most by speech-language pathologists (29, 31.2%) and nurses (21, 22.6%). The limited availability of simulation case scenarios for emergency trainings (81, 47.6%) was a concern as reported by respiratory therapists (24, 29.6%) and nurses (23, 28.4%). Additionally, onboarding healthcare professionals being time-consuming (54, 31.8%) and the lack of a standardized curriculum on tracheostomy care (49, 28.8%) were frequently cited by respiratory therapists and speech-language pathologists.
Furthermore, 27 respondents (16%) provided comments outlining other barriers to training and retaining skilled HCP in tracheostomy care. These included a lack of available HCP, staff shortages, and limited interest in achieving excellence in tracheostomy care. Some respondents highlighted misconceptions that tracheostomy care is solely the responsibility of specialists, fostering a “not my issue” attitude among routine ward staff. Other barriers included the lack of skilled specialists, inadequate bedside staff, and restrictions preventing student nurses from performing tracheostomy care due to perceived risks. Resistance among HCP to use one-way speaking valves with ventilated patients was also noted.
Additional challenges centered around insufficient funding and resources for staffing, low wages, high costs of training materials, inadequate reimbursement policies, limited time allocated for staff and patient training, insufficient time for care coordination, and the extensive time investment required for effective provider training. Further barriers included a lack of personalized training programs for families, early patient discharge from acute care settings, insufficient post-acute care resources, and a general lack of awareness regarding knowledge gaps in tracheostomy care.
Teamwork and Empowerment
Key concerns included patients and family members being inadequately empowered or engaged in decisions (73, 42.9%), reported most by speech-language pathologists (26, 35.6%) and nurses (15, 20.6%). The lack of a tracheostomy team (56, 32.9%) and personnel to support data-driven practice or benchmarking (33, 19.4%) were also highlighted, with speech-language pathologists and respiratory therapists expressing these challenges most frequently.
In free-text responses, 22 participants (13%) identified additional challenges in tracheostomy care. These included shortages of respiratory therapists, overall staffing limitations, and a lack of trained professionals within the community. Some respondents cited limited resources to expand staffing and form teams, as well as a need for tracheostomy education for nurses. Other reported barriers included insurance restrictions, inconsistent infection control practices by HCP, language barriers, and insufficient family support. Respondents also mentioned the lack of pediatric nebulizer attachments for home care, limited promotion of evidence-based practices (such as cuff deflation, swallow studies, and timely downsizing), absence of community teams for long-term care, and variations in tracheostomy management approaches. Additional concerns included a shortage of physicians with specialized tracheostomy training, inadequate support at home, and deviation from best practices to avoid the need for a second tracheostomy placement.
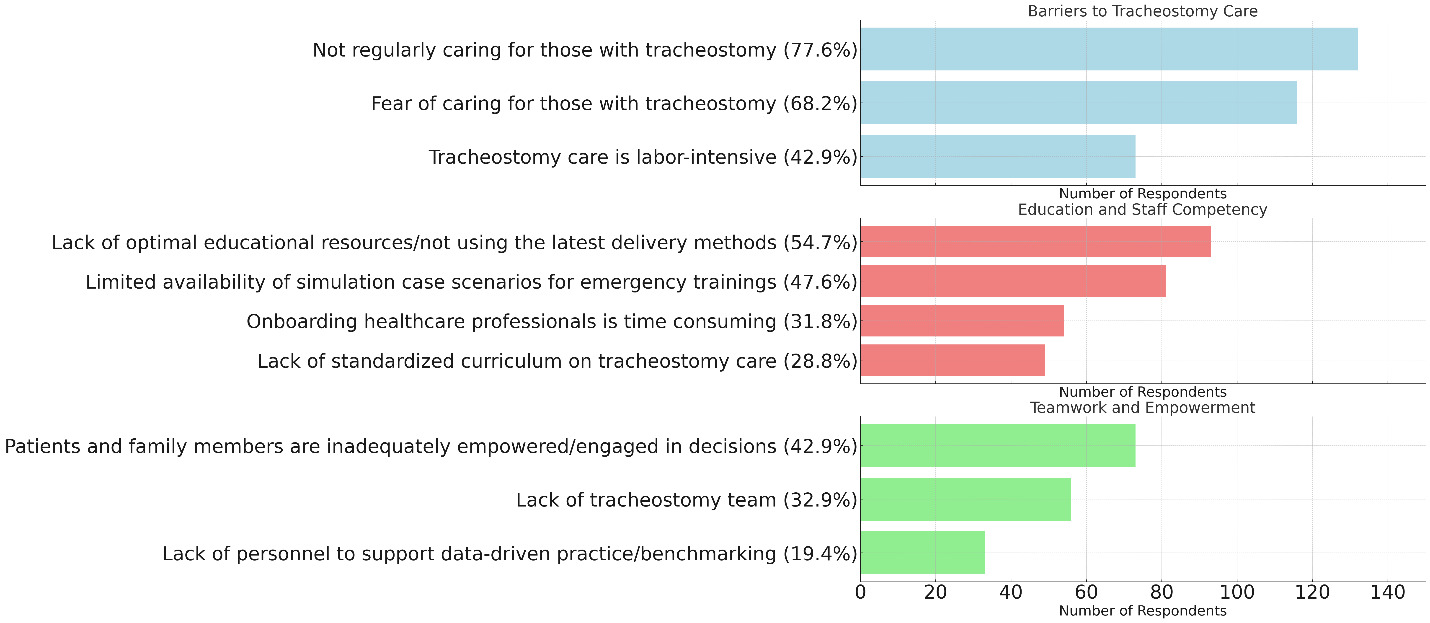
Challenges with access and affordability of tracheostomy care
The challenges related to access to and affordability of tracheostomy care were categorized by role, highlighting the diverse perspectives of administrators, family members, patients, and healthcare professionals (Figure 3; Supplemental Table 3).
Access to Care
The most frequently reported concern was access for underserved communities (99, 58%), with speech-language pathologists (35, 35.4%) and respiratory therapists (21, 21.2%) identifying this as a major challenge. Other notable issues included patient and family financial strain (86, 51%), reported most often by speech-language pathologists (23, 26.7%) and respiratory therapists (22, 25.6%). Transportation difficulties (81, 48%) and distance to travel for care (80, 47%) were also significant barriers, with speech-language pathologists and nurses highlighting these challenges, accounting for 33–34% of respondents in both cases.
Twenty-four respondents (14%) provided free-text comments on access-related concerns, which emphasized the complex interplay between tracheostomy care access and social determinants of health, financial resources, transitional care complexities, and community involvement. Commonly mentioned themes were barriers related to health insurance, coordination of care, workforce availability, and community investment. Respondents cited underinsurance, language barriers, a lack of educational materials in multiple languages, systemic healthcare disparities, misalignment of care pathways, limited access to trained professionals in community settings, and a shortage of specialists willing to provide long-term tracheostomy care.
Other concerns included inadequate discharge education, insufficient home support post-discharge, inappropriate discharge placements, limited funding for community-based tracheostomy services, and shortages of private-duty nurses and respiratory therapists. Respondents also noted inconsistencies in care standards between hospitals and community settings, and limited access to supplies from durable medical equipment providers. Family-related stressors, such as parental work commitments and health issues affecting other family members, were also identified as factors complicating access to tracheostomy care.
Affordability
Affordability challenges were led by costs in the community, including supplies, equipment, and loss of income (126, 74%). Speech-language pathologists (38, 30.2%) and respiratory therapists (34, 27.0%) reported these issues most frequently. Prolonged length of stay costs (108, 64%) were highlighted by nurses (28, 25.9%) and speech-language pathologists (34, 31.5%). Similarly, readmission costs (77, 45%) and ventilator-associated pneumonia/complication costs (76, 45%) were major concerns, with speech-language pathologists and respiratory therapists reporting the highest proportions (up to 39.5% for complications).
Additionally, 17 respondents (10%) shared further concerns in free-text responses, such as inadequate insurance coverage for tracheostomy care and medications, challenges in securing long term acute care hospital or skilled nursing facility placement for underinsured patients, lack of care options for undocumented individuals, and limited government funding. Respondents also mentioned barriers such as Medicaid expansion refusal in certain states like Texas, a shortage of facilities accepting diverse patient needs, lack of fiberoptic evaluation in rehab centers, high caretaker costs, scarcity of community support for consumable supplies, family travel burdens, and the heavy caretaking load associated with tracheostomy management.
DISCUSSION
This study identifies critical gaps in tracheostomy care, emphasizing the need for systemic improvements in workforce competency, access and affordability, teamwork, and patient empowerment. Despite the life-sustaining benefits of tracheostomy, significant challenges persist in delivering safe, equitable, and effective care. These gaps reflect the multifaceted nature of tracheostomy management, which spans diverse professional roles and care settings, often requiring collaboration among multidisciplinary teams. The findings emphasize the pressing need for targeted interventions to address these barriers, ensuring that patients, care partners, and HCPs are adequately supported in managing the complexities of tracheostomy care.
Tracheostomy care strategies must align with local circumstances, including the patient volume and specific characteristics of the healthcare setting. Small community hospitals with lower patient census, for instance, may rely more heavily on champions to prioritize competency in high-priority skills among health professionals involved in tracheostomy care, whereas large academic centers may have infrastructure to support more comprehensive tracheostomy expertise and staffing. Differences in care settings reflect the importance of adaptable care models and resource-sharing initiatives to support facilities with limited capacity for maintaining specialized trach care teams. As a result, scalable models of education and mentorship should be developed to equip smaller hospitals with essential skills while leveraging larger centers for specialized consultation and training opportunities.
Workforce Competency and Education Gaps
The most pressing concern identified was the limited availability of HCPs with specialized tracheostomy expertise, with a median severity score of 8 (IQR: 6–10). Nearly half of respondents cited a lack of optimal educational resources and emergency training scenarios, while others emphasized the absence of a standardized curriculum for tracheostomy care. Speech-language pathologists and respiratory therapists were most likely to report these challenges, reflecting their frontline roles in managing complex tracheostomy cases. Barriers to competency were compounded by staff shortages, high training costs, and insufficient opportunities for ongoing education. Resistance to adopting evidence-based practices, such as one-way speaking valves or cuff deflation, further hindered improvements in care delivery.
The fear and lack of experience among caregivers for tube changes, as well as the inadequate training for HCP, complement prior research focusing on the importance of caregiver training and support networks.33–35 These issues further highlight the need for comprehensive educational interventions that address both HCP and caregiver preparedness. In addition, retention of experienced nurses and staff plays a vital role in promoting comfort and competency in tracheostomy care.36 Without adequate retention strategies, the healthcare system risks exacerbating workforce shortages and losing valuable expertise critical to managing complex tracheostomy cases.
Addressing suctioning-related tracheostomy concerns
One area where the lack of workforce competency and standardization was particularly evident was suctioning-related tracheostomy care. Suctioning is a critical component of tracheostomy management, essential for maintaining a clear airway, preventing respiratory complications, and ensuring patient comfort. However, inadequate suctioning practices may lead to serious complications such as aspiration, infection, or even respiratory distress. While a prior study mentioned issues with stoma placement,37 our study revealed specific concerns around suctioning practices, including technique variation, patient discomfort, and inconsistent training across disciplines. These gaps highlight the broader issue of inadequate training resources and the absence of standardized education, which further compound challenges in care delivery.
Addressing these concerns requires the implementation of standardized suctioning competencies for all HCPs, including nurses, respiratory therapists, physicians, and speech-language pathologists, as well as for patients and care partners.38 These competencies should be incorporated into onboarding programs, evaluated regularly through simulations, and integrated into discharge protocols.39,40 Standardizing suctioning techniques is not only vital for improving patient safety but also represents a critical step in reducing variability and enhancing the overall quality of tracheostomy care. Structured pathways and evidence-based care protocols, as recommended by respondents, could further streamline care delivery, improving both efficiency and coordination across multidisciplinary teams.
Addressing lack of standardization in tracheostomy care
Building upon the need for standardized suctioning practices, our findings also emphasize the importance of broader standardization in tracheostomy care. Beyond suctioning, respondents identified critical gaps in the use of one-way speaking valves and delays in decannulation as areas where standardization could significantly improve patient outcomes. Studies have demonstrated that well-orchestrated tracheostomy teams can accelerate time to speaking, eating, and decannulation, highlighting the interconnected benefits of competency-based education, evidence-based practice, and quality improvement.20,21,41,42 Recent research corroborates the value of educational interventions in improving confidence, knowledge, and competency among HCP involved in tracheostomy care.43 These findings emphasize the urgent need for structured pathways and continuously refined protocols to ensure consistent, high-quality treatment across diverse care settings.44 By addressing these gaps in suctioning techniques and overall care processes, the healthcare system can reduce variability, streamline care coordination, and improve outcomes for tracheostomy patients.
Access and Affordability
Issues related to access to tracheostomy care for underserved communities were another significant concern, with 58% of respondents highlighting barriers to care. Geographic factors, such as the distance to care facilities and transportation difficulties, disproportionately affected rural and low-resource populations. Respondents also emphasized systemic inequities in healthcare delivery, including disparities in resource availability and workforce distribution. Affordability challenges ranked closely behind access issues, with costs associated with community care (74%) and prolonged hospital stays (64%) being the most frequently cited. Speech-language pathologists and respiratory therapists identified financial burdens as a critical issue, emphasizing the strain on patients and families. Respondents reported inadequate insurance coverage, insufficient funding for community-based services, and high out-of-pocket expenses, further highlighting the need for systemic changes in healthcare financing.
Although respondents were queried separately regarding access to care and financial constraints, these aspects of care are often intertwined, potentially mediated by social determinants of health. For example, economic hardship can limit access to transportation or exacerbate geographic barriers, reducing availability of specialized tracheostomy care. These interconnected challenges highlight the need for addressing both financial and structural factors that impede equitable care. By adopting a more integrated approach to financial and structural interventions, healthcare systems can better address disparities and develop sustainable solutions that facilitate long-term access to quality tracheostomy care.
These financial and access barriers exacerbate the broader challenges in tracheostomy care. Addressing these financial burdens requires targeted policy changes and systemic interventions. The financial burden associated with tracheostomy care, including costs related to supplies, equipment, and prolonged hospital stays, mirrors findings from other studies that indicate affordability remains a significant barrier to optimal care.45 The additional emphasis on inequitable access for underserved communities reported in our study further supports the call for policy changes to address these disparities and improve resource distribution. Efforts should prioritize addressing the specific needs of underserved communities, with an emphasis on improving access to essential resources and care. Limited access to supplies due to financial constraints represents a fundamental issue that requires urgent policy and systemic interventions.
Teamwork and Collaboration
Challenges related to teamwork and interdisciplinary collaboration were significant, with respondents reporting the absence of dedicated tracheostomy teams and personnel to support data-driven care. A lack of coordination among HCP was frequently noted, hindering efforts to standardize care and reduce variability in practices. Respondents also cited limited community resources and inconsistent infection control practices as barriers to effective teamwork. These findings highlight the need for targeted interventions that prioritize collaboration and foster cohesive care strategies.
Building on these insights, interprofessional collaboration emerges as a pivotal solution to address these challenges. Previous studies have identified similar barriers to effective tracheostomy management, including a shortage of HCP with adequate tracheostomy knowledge,46,47 inadequate training and support for caregivers,17 and difficulties accessing care,48 which align with the findings of our study. However, unlike previous research that has primarily focused on clinical outcomes, our study provides a holistic view by incorporating perspectives from a diverse group of interprofessional stakeholders including speech-language pathologists, nurses, respiratory therapists, patients, caregivers, healthcare administrators, and social workers. This comprehensive approach adds depth to understanding tracheostomy care challenges and emphasizes the need for interventions that address not only clinical gaps but also caregiver education and resource allocation.
Tracheostomy care spans several disciplines, necessitating broad stakeholder engagement, as emphasized during the COVID-19 pandemic era.49,50 The critical role of interprofessional teams is increasingly recognized,19 along with the significant contribution of the larger community in supporting tracheostomy care domestically and internationally.51 By implementing dedicated interprofessional teams, healthcare systems can enhance communication, streamline collaborative decision-making, and reduce barriers to effective tracheostomy care. These teams can ultimately mitigate adverse outcomes, promote consistent practices, and improve the quality and safety of care for tracheostomy patients.
Patient Empowerment and Family Engagement
Although rated lower in severity, issues related to patient and family empowerment remain critical to effective tracheostomy care. Respondents identified the absence of tailored educational resources and inconsistent discharge planning as key barriers to enabling patients and caregivers to actively participate in care decisions. These challenges are compounded during the transition from hospital to home care, a period marked by difficulties in navigating home nursing, coordinating with durable medical equipment providers, and preparing for emergencies.52 Without proper support, families often feel overwhelmed, which can compromise both caregiver well-being and patient safety.
Effective educational tools, such as pictorial handouts, have shown promise in improving caregiver confidence and reducing anxiety in managing tracheostomy care. One study demonstrated that these visual aids significantly enhance self-efficacy in both patients and family members, making them a practical intervention for addressing caregiver education gaps.53 Similarly, another study highlighted the importance of developing self-management skills for tracheostomy care at home.54 Their scoping review identified key dimensions of self-management, including managing the therapeutic regimen, navigating role and behavior changes, and addressing emotional stressors. Placing the patient at the center of self-management tasks reinforces the importance of empowering individuals and families with the skills and knowledge needed for effective home care.
Additionally, social determinants of health, including limited access to supplies, home nursing, and insurance coverage, disproportionately affect vulnerable populations, exacerbating caregiver challenges.55 Addressing these systemic barriers requires coordinated policy changes and greater investment in equitable healthcare solutions. Finally, providing emotional and psychological support for caregivers is essential. Structured interventions, such as standardized care packages and multidisciplinary collaboration, can empower families and improve both the quality of life for caregivers and tracheostomy outcomes for patients.56
Implications for Practice and Policy
These findings reveal the interconnected nature of tracheostomy care challenges, emphasizing the need for systemic changes in policy, practice, and resource allocation. Addressing the severe gaps in workforce competency requires targeted investments in training, recruitment, and retention. Similarly, improving access and affordability necessitates advocacy for equitable healthcare funding and expanded insurance coverage. Efforts to promote teamwork and patient empowerment should focus on building dedicated tracheostomy teams, enhancing care coordination, and integrating families into decision-making processes. Tailored interventions, informed by stakeholder input and evidence-based strategies, are essential for addressing these gaps and improving the quality of tracheostomy care globally.
While these recommendations apply broadly, the challenges faced in low-resource and rural settings warrant special attention. Workforce shortages, inadequate training, and limited access to care are often more pronounced in these areas, where systemic barriers are compounded by logistical constraints, insufficient funding, and lack of specialized expertise.57 For instance, access to scalable educational resources, simulation-based training, and essential supplies is frequently restricted, further exacerbating disparities in tracheostomy care.58,59 Developing tailored interventions for low-resource and rural communities is critical to ensuring equitable care delivery. These challenges highlight the need for broader systemic changes in care access and affordability, including equitable resource allocation, reimbursement policies that reduce out-of-pocket costs, and incentives to distribute healthcare professionals to underserved areas. Such policy initiatives would address existing inequities while improving outcomes for marginalized populations.
Future research should also explore the role of policy-level interventions in addressing barriers to health equity. For example, expanding reimbursement coverage for tracheostomy-related care and providing funding for tracheostomy education programs in underserved settings could bridge gaps identified in this study. Ensuring affordability and accessibility for these communities is essential to fostering global improvements in tracheostomy care.
Limitations
This study has several limitations. The reliance on the GTC Learning Community for participant recruitment, while beneficial for its multidisciplinary and international scope, may bias findings toward resource-rich settings and stakeholders involved in quality improvement efforts. The predominance of respondents from developed countries, combined with the voluntary nature of survey participation, introduces potential response bias and limits generalizability to low-resource settings. Additionally, the use of self-reported data may introduce subjectivity and recall bias. The imbalanced sample sizes between healthcare professionals (HCPs) and caregivers limited our ability to perform statistical comparisons between these groups. Instead, we focused on descriptive data to ensure transparency and avoid misrepresenting findings. Future research should recruit a more geographically diverse and representative sample, particularly from resource-limited regions, and include healthcare professionals, patients, and caregivers. Complementary methods, such as semi-structured interviews and longitudinal studies, could provide deeper insights and evaluate the long-term effectiveness of proposed interventions.
Future Directions
Our findings highlight the need for enhanced educational resources and standardized training programs in tracheostomy care. Developing simulation scenarios and readiness tools can better prepare HCPs for emergencies and routine care, particularly in underserved communities.60 Pilot programs using high-fidelity mannequins or interactive e-learning platforms can serve as practical starting points, focusing on critical skills such as suctioning, stoma care, and emergency management. These initiatives could be integrated into nursing and respiratory therapy curricula and evaluated for their impact. Innovative technologies like virtual reality (VR) and augmented reality (AR) hold promises for accelerating training and improving competency. However, barriers such as high costs, infrastructure needs, and accessibility in low-resource settings must be addressed. Scalable solutions, including partnerships with technology developers and pilot programs to evaluate cost-effectiveness, will be essential to ensure equitable adoption. Short-term, simulation-based approaches remain a practical foundation for future advancements. Finally, integrating artificial intelligence into education and clinical practice is an evolving opportunity, and equitable access must be prioritized to alleviate financial burdens on patients and caregivers. Ensuring accessibility in underserved communities is critical to making these innovations broadly impactful.
Conclusion
This study highlights critical challenges in tracheostomy care, including workforce shortages, inequitable access, affordability issues, and gaps in caregiver support. Addressing these issues requires urgent action, starting with the development of scalable, standardized training programs to enhance workforce competency. Policymakers and healthcare leaders should prioritize equitable resource allocation to improve access to care and alleviate financial burdens on patients and caregivers. Expanding simulation-based training and piloting innovative educational technologies, such as VR/AR, can provide immediate solutions while paving the way for long-term advancements. Collaborative, interdisciplinary approaches remain essential for ensuring quality and safety in tracheostomy care. Future initiatives should focus on fostering partnerships among stakeholders, including healthcare providers, caregivers, and policymakers, to implement these targeted interventions and bridge gaps in care delivery, particularly in underserved communities.
Funding
This work was supported by the Center for Immersive Learning and Digital Innovation: A Patient Safety Learning Lab advancing patient safety through design, systems engineering, and health services research (AHRQ R18 - HS029124, PI Vinciya Pandian)
Disclosures
None
Acknowledgements
The authors extend their sincere gratitude to all individuals with tracheostomies, their care partners, and the healthcare professionals within the Global Tracheostomy Collaborative for their contributions to this study. Their participation and insights were instrumental in advancing this important work.