At just six months old, EJ was diagnosed with severe subglottic stenosis—a narrowing of the airway below her vocal cords. After a series of respiratory emergencies and failed attempts at minimally invasive treatments, EJ underwent a tracheostomy to secure her breathing. The procedure saved her life, but it also marked the beginning of a complex journey for her family.
EJ’s tracheostomy requires complex daily care, including regular cleaning, monitoring for infections, and periodic changes of the tracheostomy tube. Her care also involves multiple specialists, including a pulmonologist, speech-language pathologist, and respiratory therapist, as well as the need for durable medical equipment to maintain her airway and communication. At home, her parents balance caregiving with their jobs and rely heavily on Medicaid and the Children’s Health Insurance Program (CHIP) to cover EJ’s medical expenses. These programs provide critical support for routine pediatric care, home health services, and the specialized supplies EJ requires.
When a lapse in CHIP coverage occurred due to administrative delays, EJ’s family faced significant financial strain, having to pay out of pocket for essential tracheostomy supplies and delaying follow-up appointments with her care team. This brief interruption left them scrambling to maintain EJ’s care routine while avoiding preventable complications. They reached out to tracheostomy support groups on social media to request supplies from other individuals with a tracheostomy.
EJ’s story highlights the challenges families face when relying on state and federal programs for children with complex medical needs. Medicaid and CHIP are essential lifelines for families like EJ’s, covering services and equipment that private insurance often excludes or caps. Proposed policy changes—such as work requirements or reductions in Medicaid funding—could destabilize this fragile support system, putting children like EJ at increased risk of complications and poorer health outcomes.
EJ’s journey emphasizes the importance of health policies that ensure continuous and equitable access to care for patients with tracheostomies. It serves as a reminder of the real-world consequences of systemic gaps in healthcare coverage and policy.
Introduction
The health policy implications of shifting political leadership in the United States have potentially far-reaching consequences for pediatric and adult patients with a tracheostomy. Patients, care partners, and health professionals face complex challenges, ranging from children needing access to specialized services such as speech therapy and home nursing to adults managing chronic conditions like airway stenosis, pulmonary disease, or neurological disorders.1–3 For all stakeholders, access to coordinated, long-term care is essential to maintaining health, fostering independence, and preventing complications. However, longstanding systemic barriers—such as affordability, inequities, and coverage gaps—can jeopardize this care.4,5 We describe how evolving policies may affect tracheostomy patients, their families, and the interprofessional teams dedicated to their well-being.
The Affordable Care Act (ACA) expanded healthcare access, reducing the uninsured rate from 16% in 2010 to a historic low of 8% in 2024.6,7 Table 1 provides a detailed comparison of how Medicaid, CHIP, Medicare, and ACA-related policies influence care access for tracheostomy patients, identifying both progress and gaps. Medicaid expansion and ACA marketplaces have improved access to care for many patients requiring tracheostomy care, enabling millions to utilize services such as respiratory therapy, home health care, and durable medical equipment.8 For tracheostomy patients, the continuity of such services often determines health outcomes, quality of life, and survival. However, despite this progress, approximately 1.5 million adults remain uninsured in the ten states that have not adopted Medicaid expansion.9 A lack of coverage limits access to essential care, increasing reliance on emergency services.8 This gap is particularly evident in pediatric patients, whose families often rely on Medicaid or the Children’s Health Insurance Program (CHIP) to cover their complex medical needs. Uneven implementation of CHIP exacerbates disparities in access for low-income and minority populations.10,11
Medicare’s Role and Challenges
Medicare serves as a foundation for older adults with tracheostomies, but adhering to manufacturer recommendations for replacing tracheostomy tubes, speaking valves, or humidifiers may not be covered, leaving patients at risk of suboptimal care. Traditional Medicare also excludes supplemental benefits such as hearing aids, dental care, and vision care—services integral to comprehensive patient management.12 For tracheostomy patients, these exclusions result in higher out-of-pocket expenses, compounding the financial strain on individuals and families already managing costly medical regimens.13
While Medicare Advantage (MA) plans offer expanded benefits, these policies introduce new challenges for complex patients, particularly those with a tracheostomy.14 These plans often prioritize profits over patient care, employing narrow provider networks, preauthorization requirements, and aggressive cost-control mechanisms that delay or deny access to essential services, such as tracheostomy tube changes or respiratory therapy.6,15 Moreover, overcoding practices inflate costs without improving care quality, undermining the intended benefits of MA plans.12 Addressing these inefficiencies is critical to ensuring that tracheostomy patients receive timely and coordinated care.
Efforts to reform Medicare policies, such as enhancing traditional benefits or improving competition among MA plans, hold promise but must be carefully implemented.15 For instance, increasing competition could incentivize innovation in care delivery, potentially improving outcomes for tracheostomy patients. However, without robust safeguards, such reforms risk shifting costs to patients or limiting access to specialized care.16 Policies must strike a balance between cost containment and equitable access to meet the needs of our community of individuals with tracheostomies.8
Administrative Barriers and Medicaid Eligibility Policies
The challenges are potentially even greater for the pediatric population, where parents often struggle to balance work with the demands of providing intensive care for a child during both day and night.8,17 Proposals to implement Medicaid employment mandates present significant obstacles for tracheostomy patients, who frequently require extensive and continuous care. Physical limitations, frequent medical appointments, and reliance on caregivers make it nearly impossible for many care partners to comply with such requirements.7 These policies could lead to coverage disruptions, worsening health disparities, and increasing rates of avoidable hospitalizations, infections, and mortality.8
Families already bear significant caregiving and financial burdens.4,17,18 Medicaid coverage often provides the critical support needed to access home health services and manage employment responsibilities.19 However, in states without Medicaid expansion, employment-based eligibility rules disproportionately affect low-income families, exacerbating inequities in care access.20 For example, the administrative complexity of verifying employment or tracking exemptions can deter eligible individuals from maintaining coverage, destabilizing care for tracheostomy patients.
Healthcare teams also experience significant strain under such policies. Social workers and case managers, who play essential roles in navigating Medicaid eligibility and ensuring continuity of care, face increased workloads due to the administrative demands of employment-linked eligibility policies. This phenomenon, often referred to as “Medicaid churn,” disrupts coverage for vulnerable patients, resulting in poorer outcomes and higher healthcare costs.21,22 Addressing these challenges requires policies that minimize administrative barriers and prioritize equitable access to essential healthcare services.
Structural Health Inequities
Low-income and minority populations are disproportionately affected by policy changes that impact access to or coverage of healthcare.23 Black and Native American communities face systemic barriers to accessing specialized care, perpetuating cycles of poorer health outcomes and higher rates of complications.24,25 Geographic disparities further exacerbate these inequities, as rural patients often lack proximity to specialists and critical resources.25,26
Efforts to address these disparities through Medicaid waivers targeting social determinants of health show promise. For instance, waivers that fund home-based care or provide transportation services improve care continuity and reduce preventable complications for tracheostomy patients.27 However, sustaining these programs requires bipartisan legislative support and consistent funding.28 Without these safeguards, Medicaid waivers risk being underutilized, leaving vulnerable populations without the support they need.
The recent overturning of the Chevron Doctrine introduces additional challenges by transferring interpretative authority from federal agencies to the courts.29 This shift undermines the ability of agencies like the Centers for Medicare and Medicaid Services (CMS) to implement patient-centered policies effectively.30 For tracheostomy care, this legal precedent could delay critical policy adaptations, hindering efforts to reduce health disparities. Collaborative approaches that prioritize patients’ needs in decision-making processes are essential to mitigating these systemic barriers.
Implications for Healthcare Teams
Physicians, nurses, and allied health professionals must navigate policy shifts that often disrupt care delivery, creating additional barriers to timely and coordinated interventions.31 Healthcare teams play a pivotal role in managing the complex needs of tracheostomy patients, ensuring continuity of care across various settings.32,33 For tracheostomy patients, such disruptions can lead to preventable complications, including airway blockages, respiratory infections, and hospital readmissions. Social workers and case managers act as crucial navigators, addressing gaps in care and connecting patients with essential resources.34 However, complex eligibility criteria and limited workforce capacity strain these roles. As administrative burdens grow, healthcare teams are forced to prioritize acute needs, leaving many tracheostomy patients without proactive care coordination.
These challenges also affect the broader healthcare ecosystem. Nurses, respiratory therapists, speech-language pathologists, social workers, and physicians continually grapple with time constraints. These healthcare professionals and families often bear the brunt of administrative inefficiencies, diverting attention from direct care. The resulting burnout contributes to workforce shortages, jeopardizing the quality of care for tracheostomy patients. Addressing these issues requires investments in care coordination infrastructure, streamlined administrative processes, and increased support for case management services.
Advocacy and the Path Forward
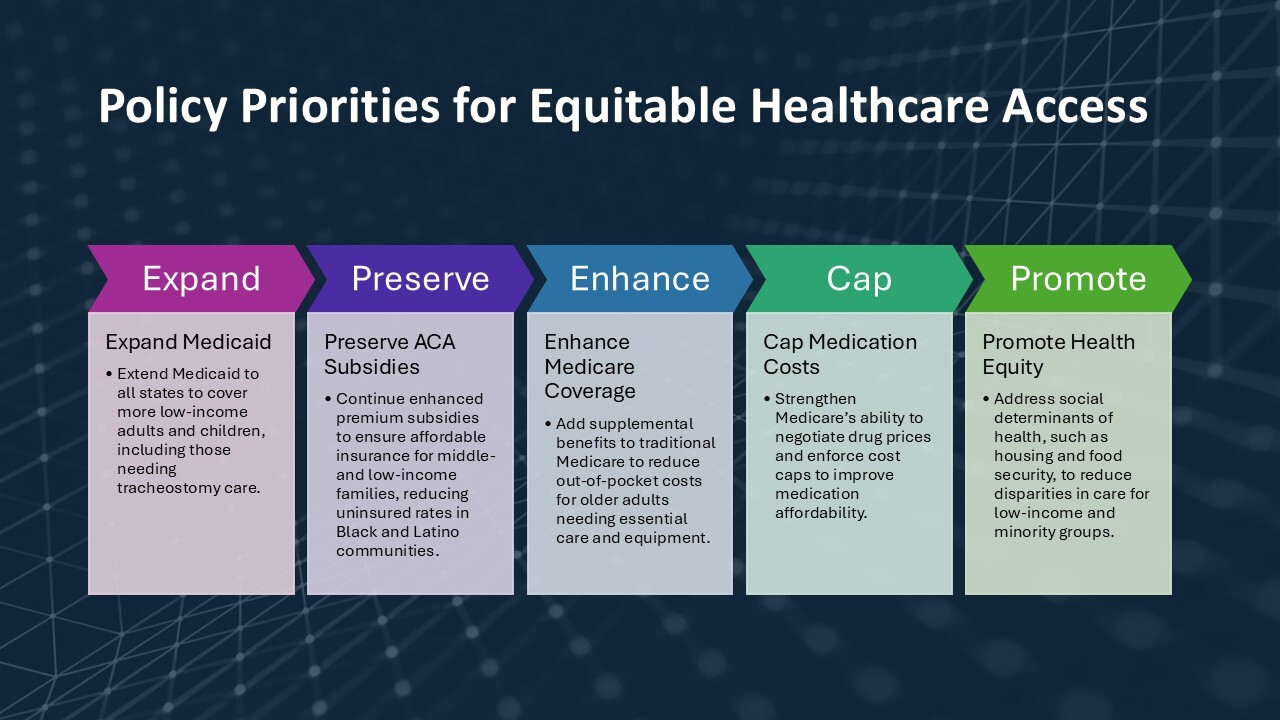
Advocacy is essential to addressing the systemic barriers that impact tracheostomy patients, who often face high costs, complex care needs, and disparities in access. Key policy priorities for advancing equitable healthcare access are summarized in Figure 1. Priority areas include expanding healthcare coverage, reducing financial burdens, and promoting equity through reforms. Expanding Medicaid to all states would provide coverage to millions of uninsured individuals and improve access to specialized care.35 Strengthening Medicare by adding supplemental benefits would alleviate financial burdens for adults with tracheostomies, addressing critical gaps in coverage.36 Additionally, extending the enhanced ACA subsidies introduced by the Inflation Reduction Act would help maintain affordable insurance options for middle- and low-income families, preventing catastrophic financial burdens.37 Addressing social determinants of health, such as housing, food security, and the digital divide, can reduce disparities and improve outcomes for vulnerable populations.24,29,38
Conclusion
The results of the 2024 election could significantly shape healthcare access for tracheostomy patients and their families. Addressing systemic barriers like affordability, inequities, and care gaps is essential to ensuring high-quality, equitable care. Expanding Medicaid, enhancing ACA subsidies, and improving Medicare can reduce financial burdens and disparities. Collaboration among healthcare professionals, policymakers, and advocates is vital to driving reforms that prioritize equity, streamline care, and address social determinants of health. By seizing this pivotal moment, we can create a healthcare system that ensures every patient receives the care they need and deserve.
Funding
Center for Immersive Learning and Digital Innovation: A Patient Safety Learning Lab advancing patient safety through design, systems engineering, and health services research, PI: Vinciya Pandian (5R18HS029124)
Disclosures/Conflicts of interest
none