Introduction
Emergency care physicians are often called upon to provide care for patients in respiratory distress, and managing difficult airways is a critical aspect of Emergency Medicine.1 A difficult airway arises when an experienced airway provider is unable to ventilate or intubate using direct laryngoscopy.2–4 Research has reported a 2.3% incidence of difficult airway in operative settings,5 with some limited evidence suggesting higher rates of up to 10.3% in areas outside of the operative room.6 Although some literature suggests a low rate of failed intubation in the emergency department (ED),7 failure to intubate the trachea on the first attempt occurs in 20-30% of tracheal intubations performed in the emergency department or intensive care unit (ICU) and is associated with increased risk of adverse events, including life-threatening complications.8–11
Implementing multidisciplinary difficult airway response teams (DART) has been associated with improved first-attempt success rates and increased rapidity in securing difficult airways, but most of this work has been conducted in the inpatient setting.12–14 Therefore, little is known about the feasibility and outcomes of implementing DART programs in the emergency department setting. Videolaryngoscopy, fiberoptic scopes, and other advanced airway techniques are often used by DART teams.13 A recent randomized trial found that use of a video laryngoscope resulted in a higher rate of successful first-attempt tracheal intubation than the use of a direct laryngoscope among critically ill adults in an emergency department or ICU,15 consistent with other work showing benefit of video laryngoscopy in other settings.16,17 Other trials have considered the role of bougies or fluid bolus on intubation outcomes,18–20 but little is known about outcomes of DART in the ED setting.
Patients requiring difficult airway management in the ED are often medically complex, have high acuity, and possess limited pulmonary reserve. Therefore, a multidisciplinary team-based approach might allow health care professionals with complementary expertise in airway securement, respiratory care, and pharmacy or nursing to coordinate care. Although technology is increasingly adopted in emergency medicine, the skillset for managing different aspects of a difficult airway, may not be routinely utilized by emergency physicians.21 This study builds on our prior work with a multidisciplinary DART program for inpatient difficult airway situations.22,23 In this paper, we describe the experience of the DART program in the ED at an academic, tertiary care institution, and describe the clinical outcomes of the program.
This study aims to describe patient characteristics and event-related factors associated with DART activation and airway securement outcomes. We investigated the airway securement techniques used and predictors of first attempt success rate. Additionally, we hypothesize that advanced airway securement techniques would improve first attempt success rate compared to direct laryngoscopy.
METHODS
Study Design and Setting
The protocol was reviewed by the institutional review board and designated as a “Quality Improvement Project /Not Human Subject Research” (NA-00089582). The observational cohort tracked the experience of the DART program and its outcomes in the ED of the Johns Hopkins University Medical Center, an academic, tertiary care institution. Findings were reported based on the recommendations of the Strengthening of the Reporting of Observational Studies in Epidemiology Statement: guidelines for reporting observational studies.24,25
Implementing the Emergency Department DART Program
Developing DART for the Emergency Department was motivated by the perceived opportunity to reduce adverse airway events outside the operating room (OR). Analysis of the adverse events involving airway management in the emergency department or other settings identified contributions from inconsistent mechanisms for communication, lack of awareness on how to activate airway support, limited access to specialized airway equipment, lack of clear roles for patient safety staff when difficult airway events arose, and variable expertise with advanced airway techniques. To address these issues, the DART program was developed to identify difficult airway patients, mobilize physicians and support patient safety staff, expedite delivery of key equipment, implement airway response algorithms, document airway techniques used, and track outcomes, with feedback on airway information shared among health care providers.
The multidisciplinary DART was established as a hospital-wide patient safety initiative.21,23,26 The DART program was designed to complement existing hospital-based response teams, such as code or rapid response teams. The efforts were coordinated through the institutional Patient Safety Committee and partnering departments including Emergency Medicine along with Anesthesia-Critical Care Medicine, Otolaryngology – Head and Neck Surgery, and General Surgery. The team members included: physicians, respiratory therapists, nurses, and equipment specialists as well as a human factors engineer to identify safety hazards, a patient safety officer, a clinical coordinator to manage on-call schedules for DART members, and a risk manager.
Departments vested in the program comprised Emergency Medicine, Anesthesiology, Otolaryngology-Head and Neck Surgery (OHNS), and General Surgery. This approach allowed for synergies in the management of patients in the ED requiring specialized care. The DART process included standard protocols, training courses, standard equipment, in addition to the creation of the multidisciplinary airway management response team. Emergency physicians played a leadership role in collaborative intervention and educational efforts, serving as primary champions for rollout of DART in the emergency department setting. The role of anesthesiologists, OHNS, and General/Trauma surgeons have also been described in detail in prior publications.23,27,28
Participants
All patients aged 18 years or older managed by the DART team in the ED over a five-year period were included in the study. Thus, any instance where the DART team was activated would result in study inclusion. In contrast, patients were excluded from the study if the DART team was not activated during their care, even if an airway concern was identified and managed independently by the emergency physicians. Data was collected and analyzed only for patients in the ED where a DART activation occurred.
Intervention
The DART is activated through an emergency paging system and triage protocol. According to our institution’s policy, when a patient requires emergent airway management, the code team or rapid response team is activated first depending on the severity of the situation. These teams handle initial intubation efforts, provided the airway is not deemed difficult. However, if the airway proves complex or the code team is unable to secure the airway, the DART is then activated to manage the situation. The criteria for activating DART for adult patients include: known difficult airway (documented in electronic health record or indicated by a difficult airway wristband), or situations where standard intubation techniques fail.
As part of the DART intervention, DART carts are strategically placed throughout the hospital. The DART cart contains advanced airway management equipment including fiberoptic bronchoscope, supraglottic airway devices, Bougie, rigid laryngoscopes, and surgical airway equipment.23 The cart allows for easier access to specialized equipment during a difficult airway event. A multidisciplinary team of anesthesiologists, OHNS, and trauma surgeons were immediately available by the established hospital-based emergency response paging system 24 hours, seven days a week during a difficult airway event.23 Data related to each DART call are prospectively entered into a hospital-based quality improvement airway registry. A multi-disciplinary difficult airway course was also developed whereby emergency department personnel and partnering disciplines developed standardized algorithms for managing difficult airways.28 The algorithms were disseminated to clinicians through interdisciplinary educational sessions that utilized hands-on skills stations, high fidelity simulation, and teamwork practice.28,29
Measurements
We obtained a list of patients who required DART intervention from the institution’s Airway Registry, where data were entered in prospectively by the study team. The list was crosschecked with ED clinical databases. Data collected included patient demographics and characteristics, DART event-related factors, techniques used to establish an airway, and patient outcomes. These data were extracted and validated by the study team.
Outcomes
The primary outcome measures were the types of intubation techniques used and the need for surgical airway intervention. Direct laryngoscopy and videolaryngoscopy were classified as basic intubation techniques. However, the combination of fiberoptic bronchoscopy with or without laryngeal mask airway, as well as the use of Eschmann or Bougie in conjunction with the laryngeal mask airway, were categorized as advanced intubation techniques. Surgical airway interventions included revision of a pre-existing tracheostomy, cricothyroidotomy, or new tracheostomy. An intubation or surgical airway intervention attempt was considered successful if the patient’s airway was secured and no additional attempts were required. Secondary outcome measures included airway injury, hemorrhage, and mortality.
Analysis
Research Electronic Data Capture tool (REDCap) was used for data management30,31 Stata® Intercooled Version 14 was used to analyze the data.32 Means and standard deviations were calculated for parametric data, and frequencies and percentages were reported for categorical variables. Pearson Chi Square test were used to compare categorical variables and logistic regression analyses were performed to identify predictors of first attempt success.
RESULTS
Characteristics of Study Subjects
Ninety-eight patients met the study’s inclusion criteria. The mean age was 50±16.5 years; there were 41 women (42%) and 57 men (58%). The racial/ethnic breakdown included Black or African American (76 [78%]), Caucasian (17 [17.3%]), Asian (two [2%]), Middle Eastern (two [2%]), and Hispanic (one [1%]). The mean body mass index (BMI) of the 86 patients for whom height and weight were available was 32±12m2. Thirty-three DART patients presented to ED with pulmonary conditions (34%), 26 with angioedema (27%), 20 with trauma (20%), 12 with neurological conditions (12%), five with hemodynamic instability related to hypovolemia, cardiogenic shock, or sepsis (5%), and two with head and neck oncological conditions (2%). Twelve patients (12.2%) had a prior history of difficult airway. Seven of those 12 (58%) had a pulmonary indication for intubation.
Ten (10.2%) patients had a history of tracheostomy before DART activation; however, the replacement of the tracheostomy tube was deemed difficult in these cases. Despite the presence of a well-formed stoma, factors such as reduction in stoma diameter or changes in tissue integrity likely contributed to the complexity of tube replacement. Of these 10 patients, two had a history of a tracheostomy but no tracheostomy tube in place at the time of DART activation (one patient still had a patent stoma). The remaining eight patients had a tracheostomy tube in place during this presentation. Five of these eight patients received a tracheostomy for chronic ventilator dependence, while three received it to address an inadequate airway patency (two had subglottic stenosis and one had airway obstruction due to myasthenia gravis). Additionally, nine patients had a reduced range of motion of the cervical spine: seven had a cervical collar in place, and two had a history of surgical cervical fusion. Of the 37 patients who had airway edema, 26 (70.3%) had angioedema, while 11 (29.7%) had edema related to trauma. Five (5.1%) patients had a history of tumor and were in remission, and five (5.1%) patients had active tumors undergoing radiation to the head and neck regions or had undergone a head and neck surgery. Ten patients (10.2%) were found to have a history of chronic obstructive pulmonary disease.
DART Event-Related Factors
The most common indication for DART activation was an anticipated difficult airway, typically due to known anatomic risk factors, but without prior difficult airway events (n = 49 [50%]). The second most common indication for DART activation was a difficult airway situation that arose while in the emergency department. DART was activated for 46 patients by the ED physicians who were encountering difficulty securing a stable airway (Table 1). At the time of DART activation, cardiopulmonary resuscitation (CPR) was in progress for 13 patients. Four patients reported difficulty with ventilation.
DART evaluated 84 patients using direct laryngoscopy (22 [22%]), videolaryngoscopy (24 [24%]), or fiberoptic bronchoscopy (38 [39%]). Two patients did not receive an airway evaluation because their airways were secured before the DART arrived. Twelve patients required urgent intubation due to deteriorated clinical status and had endotracheal tube placement without a formal airway evaluation via videolaryngoscopy or fiberoptic bronchoscopy.
Eighteen patients (18.4%) from the 98 evaluated did not require airway intervention and could be managed with medications such as nebulizers or steroids or observation in the ED. Of the remaining 80 patients, 55 (56.1%) patients were definitively managed in the ED. Sixteen (20%) patients were transported to an operating room (OR) after at least one attempt to secure the airway in the ED failed; nine (11.3%) patients were transferred directly to an OR for definitive airway management. Forty-seven (58.8%) of the 80 patients who required airway securement received induction and paralytic agents. Table 1 provides information on the type of induction agents administered and the rationales for not administering a paralytic agent.
Airway Securement Techniques
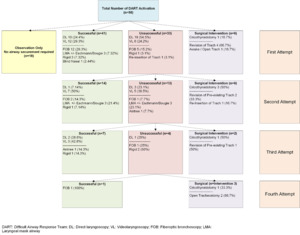
Of the 80 patients who required DART airway securement, the technique used for first attempt at securement was most often either direct laryngoscopy (28 [35%]), videolaryngoscopy (20 [25%]) or flexible fiberoptic bronchoscopy (17 [21%]) (Figure 1). Other techniques used for the first attempt included Laryngeal Mask Airway with or without Eschmann/bougie (three [3%]), rigid laryngoscope (Dedo/Hollinger) (four [5%]), or blind nasal intubation (one [1%]). The most utilized rescue techniques during all attempts were videolaryngoscopy (n = 35 [28.6%]) and direct laryngoscopy (n =36 [27.7%]). The outcomes of different techniques for managing airways are summarized in Figure 2. The first-attempt successes rates were 71% for fiberoptic bronchoscopy, 60% for videolaryngoscopy, and 36% for direct laryngoscopy. When these approaches were unsuccessful, advanced interventions were often needed, such as cricothyroidotomy or open tracheostomy.
Seventeen (21.3%) out of 80 patients required surgical airway intervention. Twelve (71%) of the 17 patients received a surgical airway intervention in the ED; five patients (29%) received a surgical airway intervention in the OR. Of these 17 patients requiring a surgical airway, seven (8.8%) patients had pre-existing tracheostomy and required a tracheostomy tube change or revision. Six patients (7.5%) underwent an emergent cricothyroidotomy. Additionally, there were three patients who were transferred to the OR where a new tracheostomy tube was placed using an open surgical technique for airway securement. The average number of attempts was 1.62±0.9; the maximum number required to establish an airway by the DART team was four attempts.
Other Clinical Outcomes
Many of the patients necessitating DART activation had complex medical conditions that resulted in soft tissue injuries, bleeding, aspiration, intensive care unit admission, or death. Few of the adverse outcomes observed were directly attributable to either primary emergency department care or the DART efforts. However, the preexisting morbidities were not always readily differentiated. For example, in four patients, there was a documentation of airway soft tissue injury noted after the DART interventions. In three of these patients, the soft tissue injury appeared to be related to the patient’s initial presentation, including a gunshot wound (n=2) or stab to the face (n = 1); however, one patient with angioedema sustained a self-limited soft tissue injury at the time of intubation in the OR.
Airway bleeding was observed in 12 patients after the DART intervention, again most often attributable to baseline injury. Five (41.7%) of these 12 patients had airway bleeding that required blood transfusion. Among these five patients, sources of bleeding included traumatic events such as a gunshot wound or stab injury. In addition, one patient had significant epistaxis associated with an underlying bleeding disorder. Seven (58.3%) of these 12 patients had blood loss from the airway that did not require any administration of blood products. Of the seven patients, three had gunshot wounds to the face, one had facial trauma related to an assault, one had cardiopulmonary resuscitation in progress, one had hematemesis associated with a variceal bleed, and another had an emergent cricothyroidotomy with associated bleeding.
Eight patients aspirated gastric contents associated with DART interventions. Three of these patients had aspiration events while receiving cardiopulmonary resuscitation. One patient had a witnessed aspiration prior to DART arrival, while in supine position during an emergent tracheostomy tube change. This patient had a difficult airway event immediately after a meal when he developed a mucus plug in his tracheostomy tube, and the respiratory therapist was unable to remove the mucus plug. In the other four patients, the timing and etiology of aspiration could not be determined.
Critical illness and mortality occurred for several patients in the cohort. After DART intervention in the ED, 77 patients (78.6%) were admitted to one of the intensive care units in the hospital. Only ten patients (10.2%) were admitted to the wards, and five patients who did not require airway intervention were monitored and discharged to home. Six patients died in the ED after an airway was established. Two patients were stabilized in the ED and admitted to the intensive care unit but died within 24 hours; three patients died between 24 and 48 hours after the DART intervention; and six patients died over 48 hours after the DART event but before discharge from the hospital. None of these deaths were attributed to airway management on external review. Of the 81 patients alive at the time of discharge, six patients had a baseline brain injury that did not worsen after the DART event, and no new brain injuries were identified.
Predictors of First Attempt Success
Among 73 patients, Pearson chi-square test revealed a statistically significant association between primary diagnosis and first airway management success (χ² (6) = 16.2, p = 0.012). The association was related to the number of angioedema patients, where the majority (13 patients, 92.9%) were successfully managed on the first attempt, with only one patient (7.1%) resulting in failure (p=0.028). Most patients (71.4%) presenting with angioedema-induced airway obstruction were managed primarily using fiberoptic laryngoscopy or bronchoscopy, followed by direct laryngoscopy (14.3%).
There was a significant association between difficulty with bag-mask ventilation and the success on the first attempt of securing the airway (χ² (3) = 22.1, p = <0.0001). Patients for whom bag-mask ventilation was deemed difficult were associated with a lower rate of success on the first attempt of securing the airway compared to patients where bag-mask ventilation was not difficult. Furthermore, in patients where bag-mask ventilation was not required, the first attempt success rate was higher (39 patients, 83%) compared to failure rates (11 patients, 33.3%).
The first attempt success rate was higher among patients who did not require CPR (66 patients, 93.6%) compared to patients requiring CPR (14 patients, 6.4%). Logistic regression analysis also revealed a significant association between cardiopulmonary resuscitation being in progress at the time of airway securement attempts and success on the first attempt of securing the airway, controlling for their primary diagnosis and difficulty with bag-mask ventilation (χ² (1) = 9.8, p = 0.002).
Comparison of Airway Securement Techniques: Basic vs. Advanced
The overall success rate for first airway securement attempts was 56.2%, (41 successful patients and 32 patients resulting in failure) (Figure 3). The use of advanced airway techniques (fiberoptic bronchoscopy, videolaryngoscopy, or rigid laryngoscopy) accounted for 76% of first-attempt successful intubation rate versus 24% for direct laryngoscopy (χ² (1) = 7.7, p = 0.005).
DISCUSSION
Each year, over 1.5 million adults in the United States with critical illness are intubated in the emergency department, intensive care units, or other settings outside the operating room.33,34 Although only a small fraction of these intubations meet criteria of a difficult airway, first-attempts at tracheal intubation are unsuccessful in approximately a quarter of patients undergoing tracheal intubations in emergency department or ICU settings.15
On average, about 70,000 patients visit the study institution’s ED annually, and approximately 1,000 intubations are performed. Most DART activations are for anticipated or active airway emergencies associated with pulmonary conditions, angioedema, and trauma. Half of the patients requiring DART activation did not have a prior history of a difficult airway. In patients who received DART interventions, there was a frequent need for advanced airway techniques that are not widely used in routine Emergency Medicine practice. Fiberoptic intubation was the most used advanced airway technique and had a lower failure rate than other techniques. This study afforded insights into the patient population that prompted DART activation, the approaches used for airway securement, and the clinical outcomes.
Patient Characteristics
The patients in this study exhibited a wide range of underlying etiologies. Twelve percent of 98 patients presented with a prior history of difficult intubation. This suggests the need for maintaining robust and easily accessible databases to identify a previous history of difficult intubation for emergency physicians. The largest group of patients with a difficult airway had underlying pulmonary conditions, which represent a high proportion of patients requiring intubation in EDs.6,35 Patients with angioedema often underwent fiberoptic bronchoscopy.26 They comprised the second largest group of patients with a difficult airway in our study. In another large study, only 0.15% of 8,937 intubated patients in the ED had an indication of angioedema for intubation.36 The rate of angioedema in our study was likely higher than in other series because our sample was limited to patients for whom DART was activated.
Trauma was the next largest group that had a difficult airway. Most of these patients did not have a documented prior history of difficult airway but rather an active difficulty related to head and neck trauma. BMI has been reported to be a risk factor for difficult airways27; however, in our study sample, we found many patients with BMI < 35 who had a difficult airway. The history of a tracheostomy with or without an active tracheostomy tube in place was also a risk factor for difficult airway. For patients with a tracheotomy tube in place, the reason for DART activation was predominantly dislodgement of the tube that occurred prior to ED arrival and difficulty in tube replacement, possibly related to reduction in stoma diameter causing the difficulty. Clinicians may need to be aware and not overlook the potential for difficult airway in low BMI patients and in those with tracheostomy dislodgement.
Predictors of First Attempt Success with Airway Securement
Our study identified several predictors of first attempt success when securing the airway with tracheal intubation. Notably, the association between primary diagnosis and first airway management success implies that tailoring airway securement strategies based on the patient’s underlying condition may contribute to higher success rates. Specifically, the successful management of angioedema patients on the first attempt underscores the significance of use of advanced techniques such as fiberoptic laryngoscopy or bronchoscopy in airway management.
The correlation between difficulty with bag-mask ventilation and first attempt success further elucidates the complexity of airway management. Patients encountering difficulty with bag-mask ventilation exhibited lower success rates on the first attempt, emphasizing the importance of recognizing and addressing challenges associated with this bag-mask ventilation. Moreover, the higher success rates in cases where bag-mask ventilation was not required suggest the potential benefits of proactive strategies to prevent complications.
The impact of CPR on first attempt success is a critical finding in our study. The significantly higher success rate among patients not requiring CPR highlights the challenges posed by the dynamic and high-stakes environment of resuscitation scenarios. Logistic regression analysis controlling for primary diagnosis and difficulty with bag-mask ventilation verified the independent association between ongoing CPR and reduced success on the first attempt. This emphasizes the need for specialized approaches and heightened preparedness during airway securement attempts of difficult airways during resuscitation efforts.
In this study, we aimed to compare the efficacy of basic and advanced airway securement techniques, shedding light on the factors influencing the success of the first attempt in airway management. Our findings demonstrate a significant difference in the success rates between basic and advanced techniques, with the latter proving to be more successful on the first attempt. This discrepancy highlights the potential advantages of adopting advanced airway securement techniques in EDs when difficult airway is suspected.
Anticipation and Education
In our study, emergency physicians anticipated a difficult airway and activated DART in the absence of history or documentation of difficult airway. At our institution, emergency physicians received training and encouragement in calling the DART when there is concern for a difficult airway. Preemptive DART activations typically involved situations with high-risk for airway edema, including angioedema, trauma, and anaphylactic reactions.26 However, there were also patients with normal or low BMI and underlying pulmonary or neurological conditions that posed a risk for difficult airway who were appropriately identified as requiring a DART. Our experience emphasizes that difficult airway status is not solely based on airway anatomy. Several contextual factors can predispose to a difficult airway. The role of multidisciplinary team-based education is crucial to understanding and reinforcing these nuances in airway management.37,38
Value of DART
DART provides a framework for improving the organization and quality of care around emergency airways, building on prior work on difficult airway management in the ED setting. Implementing a DART team enhances not only the algorithmic and technical aspects of airway management but also encourages identification of early warning signs, thus providing an anticipatory mechanism for early activation.39,40 The DART concept aligns with the three-dimensional Emergency Medicine model of clinical practice that incorporates considerations of patient acuity; physician tasks; and components of medical knowledge, patient care, and procedural skills. These interrelated dimensions are used concurrently when providing patient care in urgent airway situations.41 Implementing team-based difficult airway management is particularly valuable in academic settings with resident physicians and is conducive to promoting development of interprofessional skills and has relevance across the career continuum.42 DART Teams can apply an evidence-based approach that incorporates difficult airway prediction tools.11,43,44 Data from this cohort and prior studies of DART show the value of bougie, video laryngoscopy, and other advanced airway techniques.19,45–49 When DART is activated, other expert clinicians who arrive do not entirely take over the patient care. Instead, there is active and collaborative involvement with the emergency physicians as part of the DART, using their expertise to create a multispecialty difficult airway management plan. Notably, 31% of patients who required difficult airway management were identified by the team as requiring transfer to the OR for difficult airway management.
In review of the techniques used for the first attempt, 56% of the patients required advanced airway skillsets not routinely part of Emergency Medicine expertise. Moreover, once the team chose an advanced airway technique, they continued utilizing advanced airway skills on repeated attempts for definitive airway management. Fiberoptic intubation had the lowest failure rate on initial attempt and did not require a transition to a new advanced airway technique. Our findings are similar to a recent study by Hayden et al. who reported a success rate of 71% with ED fiberoptic intubation.21 These similar rates would indicate that emergency physicians might consider integrating fiberoptic intubation into their airway management skillset or partnering with specialists proficient in these specialized techniques.
The topic of emergency airway management has drawn increased interest in the context of the COVID-19 pandemic, with potential implications for future respiratory pandemics. Concerns relating to viral transmission led to specialized guidelines for managing airway patients,50 specialized algorithms for emergency airway management,51 and consensus guidelines for tracheostomy management and other aerosol generating procedures.52 This study builds on prior work exploring the role of critical airway teams13,23,53 and have prompted increased adoption of video laryngoscopy and other technology that increased the distance of the operator from the patient’s mouth and airway, which might mitigate risk of viral transmission.54 As emergency airway management becomes more specialized, there may be a growing role for integrated teams.
Limitations
Difficult airway management is not conducive to study in controlled trials, and therefore this study of outcomes of implementing a DART is descriptive, relying on within-sample comparisons and previous reports. The literature suggests an incidence of 1–11% of airway injury related to intubation.6,55,56 In our study, none of the patients developed bleeding attributed to intubation, but there was one patient with mild soft tissue injury. We may not have accounted for all the airway injury in our study since we did not perform diagnostic airway evaluations post-intubation. We also cannot assess the effectiveness of DART in ED compared to conventional airway management practices.
Implications for Future Research
Future studies should explore the associations between knowledge of a prior history of difficult airway and successful airway management. Additionally, exploring the psychosocial and emotional impacts of DART activations on the ED team could provide valuable insights into reducing team trauma. To better understand the impact of DART, future studies should compare similar groups of patients with difficult airways for whom DART was activated or not, although any such study would be prone to bias in the absence of randomization. Despite challenges in equipoise design, propensity matched case-control study might alternatively afford insight into effectiveness of DARTs. Furthermore, larger sample sizes are needed to assess whether videolaryngoscopy should be used universally in DART activations, as well as to explore the potential for improved patient outcomes and reduced secondary trauma among ED staff.
CONCLUSION
Emergency physicians deemed the need for DART when patients had a history of difficult airway, anticipated difficult airway, or when they encountered difficulty upon attempting to secure the airway. Even with the presence of a DART at the bedside, patients were transported to the OR on certain occasions for definitive airway management. Advanced airway techniques such as fiberoptic bronchoscopy and video laryngoscopy were associated with improved initial success rate. Findings from this study support further investigation of team-based airway management in Emergency Medicine and support the role for training in equipment and technology that support first-attempt intubation success.
ARTICLE SUMMARY
-
Why is this topic important?
Effective management of difficult airways in the Emergency Department is crucial to reduce morbidity and mortality rates associated with airway compromise.
-
What does this study attempt to show?
The study aims to demonstrate the outcomes of an Emergency Department Difficult Airway Response Team (DART) program, emphasizing the importance of a interprofessional approach in managing challenging airways.
-
What are the key findings?
First-attempt intubation success in the DART implementation was associated with the use of advanced airway techniques (76% success) compared to direct laryngoscopy (24% success). Factors such as difficulty with bag-mask ventilation, need for cardiopulmonary resuscitation, and underlying illness were predictors of lower first-attempt success rates. No airway-related mortalities occurred, and surgical interventions, including cricothyroidotomy, were required in a subset of patients (17 cases).
-
How is patient care impacted?
The DART program provides a well-coordinated and structured response, enabling a interprofessional team to manage difficult airways promptly and effectively in the Emergency Department. Advanced airway techniques demonstrated superior success rates, suggesting potential benefits in patient outcomes when faced with challenging airway situations. Understanding the factors associated with first-attempt success, including patient characteristics and clinical context, can inform decisions on equipment selection and the need for surgical airway interventions, contributing to improved patient care.